What is Spinocerebellar Ataxia?
Spinocerebellar ataxia (SCA) is a degenerative disease caused by atrophy to the cerebellum, the part of the brain responsible for coordination of movement. Clinical features of spinocerebellar ataxia include problems with speech, swallowing, balance and coordination, along with peripheral neuropathy, and muscle stiffness.
Non-cerebellar features can also be present with SCA, including REM (rapid eye movement) sleep behaviour disorder, daytime sleepiness, chorea, cognitive deficits, weight loss, and urinary dysfunction.
An increasing number of SCA subtypes have been associated with specific genes, and are categorised numerically, beginning SCA1, SCA2, SCA3, through to SCA36. The numbers do not indicate severity of symptoms or the disease, but instead the order in which the dominant genes associated with SCA were identified.
As SCA can present as parkinsonism, especially with subtypes SCA2, SCA3 and SCA17, testing for these subtypes of SCA may be beneficial in patients with Parkinson’s disease.
What is Parkinsonism?
Parkinsonism is a clinical syndrome presenting slowness of movement, stiffness, and tremors. Parkinsonism is a term covering a range of conditions with similar symptoms to Parkinson’s disease, which is the most common form of parkinsonism, the cause of which is still unknown. There are a number of causes of parkinsonism in other conditions, including side effects from medication and environmental toxins to aging and hereditary predisposition.
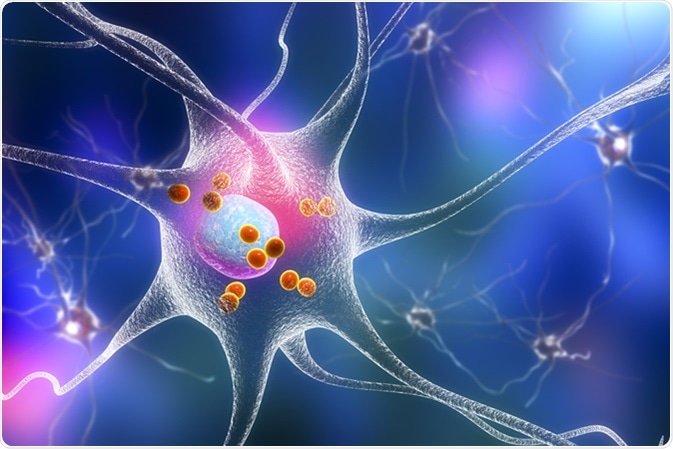
Parkinson's disease. 3D illustration showing neurons containing Lewy bodies small red spheres which are deposits of proteins accumulated in brain cells that cause their progressive degeneration. Image Credit: Kateryna Kon / Shuttertock
The clinical features of parkinsonism in spinocerebellar ataxia include:
- Cerebellar ataxia
- Dysarthria
- Tremor
- Hypoactive deep tendon reflexes
- Peripheral neuropathy
- Slow saccadic eye movement
One review has shown that after intention or postural upper-limb tremors,parkinsonism was the most common symptom concerning movement disorders at the onset of SCA.
SCA Subtypes and Parkinsonism
Parkinsonism is seen in various SCA subtypes. Levodopa-responsive Parkinson disease (PD) and atypical parkinsonism are particularly seen in SCA2, SCA3 and SCA17.
SCA2
SCA subtype SCA2 is the most commonly reported type of SCA associated with parkinsonism, and is fairly common in European populations. SCA2 has a low number of expansions and interrupted structures.
SCA3
SCA3 is common in western populations. In SCA3, atrophy of the following areas has been observed:
- Pons
- Basal ganglia
- Midbrain
- Medulla oblongata
- Multiple cranial nerve nuclei
- Thalamus
- Frontal, parietal, temporal, occipital and limbic lobes
Degeneration of the substantia nigra (a basal ganglia structure) has also been observed.
SCA6 and SCA8
Spinocerebellar ataxia subtypes SCA6 and SCA8 may present parkinsonism, but SCA6 more is more commonly seen in the form of pure ataxia. Laboratory evaluations of a 69-year-old woman with gait ataxia showed that parkinsonism associated with SCA6 is pathologically similar to idiopathic Parkinson’s disease.
SCA17
Parkinsonism in SCA17 is more commonly seen in Asian populations, and especially in Korea.
Alternative Risk Factors
While many people will have DNA repetitions seen in patients with spinocerebellar ataxia, this does not guarantee the onset of the disease at any point in life. However, those with amyotrophic lateral sclerosis (ALS), a progressive neurodegenerative disease characterized by gradual difficulties with grip, alterations in vocal pitch, fatigue, and muscle cramps and twitches, with SCA2, has been reported to pose a higher risk of parkinsonism. SCA can also involve other nervous systems and lead to various neurodegenerative diseases, and is not solely limited to the cerebellar system.
Summary
Parkinsonism is the most commonly reported symptom of spinocerebellar ataxia, and so patients who solely present parkinsonism, should also have SCA considered as a possible diagnosis. Further pathological research is necessary to fully understand why spinocerebellar ataxia can sometimes present as parkinsonism. Additionally, the geographical differences in prevalence of parkinsonism and SCA needs to be investigated further to better understand global differences in incidence and prevalence, and to form solid conclusions on the epidemiology of SCA worldwide.
Further Reading
Last Updated: Sep 24, 2022