In the current pandemic of COVID-19, many patients have reported symptoms of loss of smell and taste. The cellular basis of this phenomenon has not been satisfactorily explained so far. However, a new study published in the Briefings in Bioinformatics in August 2020 shows how this symptom is related to viral pathogenesis. Discovering which cell lines are responsible for the loss of smell would be essential to understand how to manage this infection.
Recent studies show that angiotensin-converting enzyme 2 (ACE2) and transmembrane protease serine 2 (TMPRSS2) are host components that are critical for viral entry and infection of the host cell. Tissues, where these are expressed at high levels, are susceptible to infection.
The occurrence of anosmia makes it essential to understand how the virus affects the olfactory epithelium. This includes several types of cells. The horizontal basal cells (HBCs) and the globular basal cells (GBCs) make up the basal cell population, near the basal lamina. The microvillar cells (MVCs) and sustentacular cells (SUSs) provide nutrition and mechanical support to the epithelium. The tissue also contains Bowman’s gland cells (BGCs), olfactory ensheathing glia (OEGs), immature olfactory sensory neurons, and mature olfactory sensory neurons (iOSNs and mOSNs, respectively. These latter types actually bear olfactory receptors and belong to 400 or more types.
The current paper focused on uncovering the link between the patterns of expression of these molecules on cell types within the olfactory tissue in the human host, using single-cell expression.
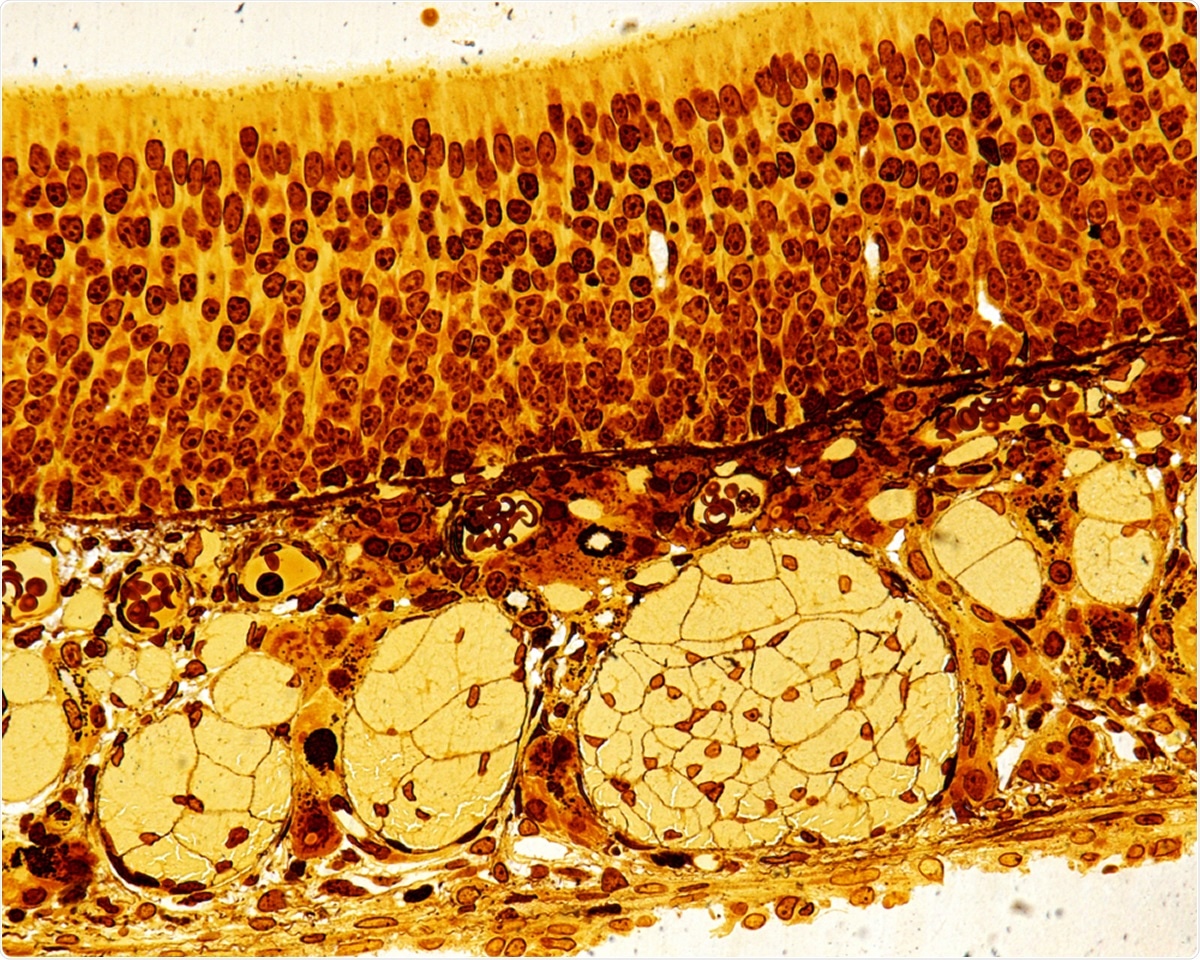
High magnification of the olfactory epithelium. The round structures of the lamina propria are bundles of axons of the olfactory nerve. Semithin resin section 0,5 µm thick stained with silver nitrate. Image Credit: Jose Luis Calvo / Shutterstock
Viral Entry Gene Expression Varies Across Olfactory Cell Types
The researchers found that ACE2 was expressed in four cell types. Namely, SUSs, BGCs, GBCs, and HBCs, but TMPRSS2 expression analysis in addition to the above showed that both were present in a subset of SUSs, which also overexpressed genes involved in cytoskeleton regulation. Some of the machinery used for viral replication of SARS-CoV was found to use intracellular transport processes linked to microtubules.
When virus-host interactions were also analyzed in conjunction with the above, they confirmed that SUSs are the most vulnerable to infection by SARS-CoV-2. This shows that even though the OSNs do not support viral entry, supporting and stem cell subsets are easily infected.
The SUSs are involved in secretion, endocytosis, and detoxification, as well as having glia-like functions like phagocytosing dead cells, and regulating ionic exchange between the inside and the outside of the cells. They are also deeply involved in communication between the nerve cells, basal cells, and the SUSs.
Various signaling pathways, including purines, phospholipase pathways, and endocannabinoids, can trigger various changes in the SUSs themselves as well as the OSNs. This could result in lowered olfactory detection thresholds, the proliferation of OSNs, with the outcome being an altered sensitivity. Moreover, any disruption in their role in the support and structural integrity of the olfactory organ could cause a loss of smell in this infection. Rodent experiments have shown that this occurs in reality.
BGCs also maintain the olfactory system in prime condition, operating through multiple mechanisms. For one, their secretion of olfactory binding proteins promotes the transfer of odorous particles to the olfactory receptor cells. They also produce mucus, a protective mechanism against the drying out of the olfactory epithelium. They also help the epithelium to repair itself rapidly following injury. When SUSs are lost, for instance, HBC activation occurs, causing them to proliferate and differentiate into new SUSs.
ACE2 Expression and ACE2-Spike Binding Comparable Across Five Mammalian Species
The researchers confirmed earlier hypotheses that other mammals, especially monkeys, can carry the virus to humans and develop anosmia when infected. They found that the olfactory epithelium in four other species of mammals carry ACE2 and TMPRSS2 at similar levels, making them vulnerable to this infection and have a similar binding affinity for the virus.
Implications
Scientists have devoted much time to making the diagnosis of COVID-19 more timely, accurate, and sensitive, as well as cost-effective. Many studies report the sudden onset of anosmia and ageusia, or at least alterations in the sense of smell and taste, before any other features of the illness. This has suggested that this symptom could be exploited as a potential tool for early diagnosis of the infection.
A symptom survey of COVID-19 patients shows that anosmia is a better predictor of infection than fever. The current study shows that this loss of smell is probably not because of damage to the OSNs. Instead, the supporting cells, namely, SUSs, BGCs, and OSCs, show the expression of molecular markers which render them susceptible to infection.
The researchers suggest that the pattern of olfactory injury is as follows: the SUSs are first infected since they are located at the apex of the olfactory epithelium, causing the olfactory epithelium to break down partly or totally, and thus resulting in an altered or lost sense of smell. This is worsened by the impaired regenerative response caused by the subsequent OSN infection.
The researchers conclude, “In light of these critical functional roles, we speculate that the apparent loss of smell could be a result of viral load in SUSs, BGCs, and OSCs.” The findings were obtained from an in silico approach, which has its limitations. This points to the need to delve deeper to detect as yet unknown host cell proteases or receptors, which may be responsible for promoting viral entry into the host cell.