Researchers in Japan and the United States have conducted a study showing that herd immunity to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) may have developed among the citizens of Tokyo during the summer.
SARS-CoV-2 is the viral agent responsible for the current coronavirus disease 2019 (COVID-19) pandemic that is continuing to sweep the globe, posing significant threats to human health.
Yasutaka Hayashida (Medical Corporation Koshikai, Tokyo) and colleagues from Boston Children’s Hospital and Beth Israel Deaconess Medical School, Boston, say their study suggests that seroprevalence for SARS-CoV-2 rose to almost 50% at around the same time cases of COVID-19 waned in the city.
“With the rise in SPR [seropositivity rate] nearing 50% within our cohort, matching the time when COVID-19 cases waned, the possibility of herd immunity should be considered, particularly in the highly-dense urban scenario like Tokyo,” writes the team.
A pre-print version of the paper is available in the server medRxiv*, while the article undergoes peer review.
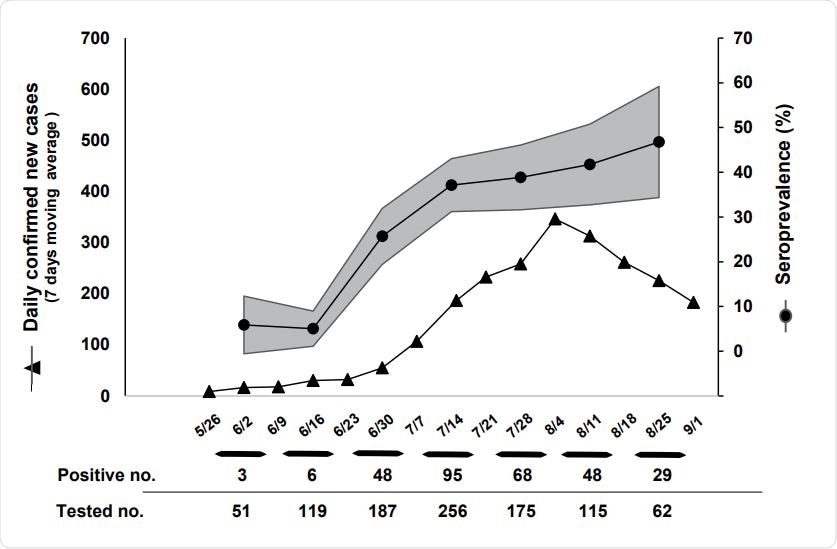
The seropositivity rate and 7 days moving average of daily confirmed new cases of COVID19 from 5/26 to 9/1
Death rate in Japan fell, despite no lockdown
Compared with the United States and European countries, COVID-19-related mortality has been low in Japan, and the death rate has fallen despite the absence of a lockdown.
The reasons for the low fatality rate are not yet known. They may be related to a low SARS-CoV-2 prevalence across the general population or decreased rates of fatality among infected cases.
Distinguishing the underlying factors requires SARS-CoV-2 prevalence data, particularly data that represent the asymptomatic general population.
“Serological tests monitored across the course of the second wave can provide insights into the population-level prevalence and dynamic patterns of COVID-19 infection,” writes the team.
What did the current study involve?
To estimate seropositivity for SARS-CoV-2 throughout the summer, the team enrolled 1,877 healthy, asymptomatic employees of large company from 11 disparate locations across Tokyo.
Across the company, serology tests for SARS-CoV-2-specific immunoglobulin G (IgG) and IgM antibodies were performed weekly between May 26th and August 25th, 2020. This time window incorporated the well-documented “second wave” of COVID-19 that occurred in Japan.
To estimate seroconversion and seroreversion among the general population in Tokyo over time, the tests were offered to each participant twice, separated by around a month.
The seropositivity rate was calculated by pooling data from each two-week window across the cohort. Changes in immunological status against SARS-CoV-2 were determined by comparing results between two test results obtained from the same participant.
Six hundred fifteen individuals, aged a mean of 40.8 years, underwent one test, and 350 of those (aged a mean of 42.5 years) underwent two tests.
Seropositivity dramatically increased over the summer
The seropositivity rate increased from 5.8% at the beginning of the study to an unexpectedly high 46.8 % by the end of the summer.
“A high seropositivity rate in Tokyo may not be fully unexpected given its remarkably high population density, tight spacing, the widespread use of public transportation, and no implementation of a lockdown,” say Hayashida and colleagues.
Of the 350 individuals who underwent both tests, 54 (21.4 %) of 252 who were initially seronegative were seropositive by the time they completed the second test. Of the remaining 98 individuals who were seropositive on initial testing, 12 (12.2%) became seronegative.
“Seroreversion was not infrequent, seen in 12% of participants over the one-month span between tests,” says the team. “This suggests that serological testing may significantly underestimate past COVID-19 infections, particularly when applied to an asymptomatic population.”
The findings can be generalized to the broader metropolitan area
The researchers say that although the study cohort was not selected from a broader, random population sample in Tokyo, the findings can still be generalized to the greater metropolitan area for a number of reasons, including the multiple disparate locations participants were from and the limited physical contact they had with each other.
Furthermore, the exclusion of symptomatic individuals could potentially have led to an underestimation of the overall seropositivity rate.
The possibility of herd immunity should be considered
“COVID-19 infection may have spread widely across the general population of Tokyo despite the very low fatality rate,” say Hayashida and team.
Although Japan took the atypical step of not implementing a mandatory lockdown, the second wave peaked and subsided nevertheless, they add.
“Given the temporal correlation between the rise in seropositivity and the decrease in reported COVID-19 cases that occurred without a shut-down, herd immunity may be implicated,” suggest the researchers.
“Future studies may consider evaluating whether lifestyle/habits, viral strain, the widespread use of masks, or host factors such as immunological memory are responsible for the observed low fatality,” they conclude.

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
Journal reference:
- Preliminary scientific report.
Hayashida Y, et al. Dynamic Change of COVID-19 Seroprevalence among Asymptomatic Population in Tokyo during the Second Wave. medRxiv, 2020. doi: https://doi.org/10.1101/2020.09.21.20198796