While the development of vaccines against the severe acute respiratory syndrome coronavirus disease 2019 (SARS-CoV-2) was welcomed by the majority of individuals around the world, some concerns have been raised regarding their potential side effects. The AstraZeneca vaccine ChAdOx1 nCoV-19 vaccine, in particular, received extensive media attention, especially in continental Europe, following reports of adverse thrombotic events.

Study: Risk of death following SARS-CoV-2 infection or COVID-19 vaccination in young people in England: a self-controlled case series study. Image Credit: Studio Romantic / Shutterstock.com

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
About the study
For the current study, data was gathered from the Office for National Statistics and the National Immunisation Management Service (NIMS), as well as an extract from National Health Service (NHS) point-of-care data. This included death registration data, as well as most of the coronavirus disease 2019 (COVID-19) vaccinations that were administered in England since December 8, 2020.
As the vaccination records of some individuals who died shortly after receiving the vaccine may not have been recorded, data was supplemented using a special extract consisting of individuals who died following vaccination without their data becoming recorded in NIMS. Linkage was constructed using NHS numbers, whereas the relative incidence of death following infection was calculated using national testing data from hospitals and in-community tests.
Any individuals who died within 12 weeks of having received a dose of the COVID-19 vaccine, as long as they were between 12 and 29 years old on this date, were included in the current study. A separate analysis included all unvaccinated individuals who died within 12 weeks of having received a positive SARS-CoV-2 test who were between 12 and 29 years of age on the date of the test.
The main exposure was time since the most recent COVID-19 vaccination before death, whereas the second exposure was time since the date of a positive SARS-CoV-2 test. Analyzed outcomes included cardiac death within 12 weeks of vaccination/positive test or death due to any cause within 12 weeks of vaccination/positive test.
To assess any change in risk of death soon after vaccination as compared to after vaccination, a self-controlled case series design was used. Follow up started on the date of the last vaccination received and participants were monitored for 12 weeks after this point.
The first six weeks were categorized as the risk period, as myocarditis normally appears very quickly after vaccination. The following six weeks were categorized as the baseline period.
Self-controlled case series models were fitted using a conditional logistic regression model on a person-week level dataset. Similar analyses were used for deaths following a positive SARS-CoV-2 test.
Deaths that occurred in later calendar weeks are less likely to be registered if there are delays in the process, which can affect follow-up weeks after vaccination, an effect that is particularly apparent for young individuals. This was mitigated by reducing the follow-up time to 12 weeks after vaccination and conducting sensitivity tests to assess the number of weeks off during the baseline period.
Study findings
A total of 585 deaths were recorded within 12 weeks of receiving a COVID-19 vaccine, 105 of which were due to cardiac events. About 46% of those who died were between 25 and 29 years of age, whereas 61% were male.
A total of 212 deaths occurred following a positive SARS-CoV-2 test, 22 of which were due to a cardiac event. It should be noted that the authors of the current study did not include the total number of individuals who were examined for each category.
Following examination of the relative incidence of both categories of deaths, the results showed that there was no evidence of change in the risk of cardiac deaths in the first six weeks after vaccination, with the relative incidence resting at 0.99. Similarly, there was no evidence of change in the risk of any deaths in the first six weeks following vaccination, and a reduction in the risk of death for the first week following vaccination.
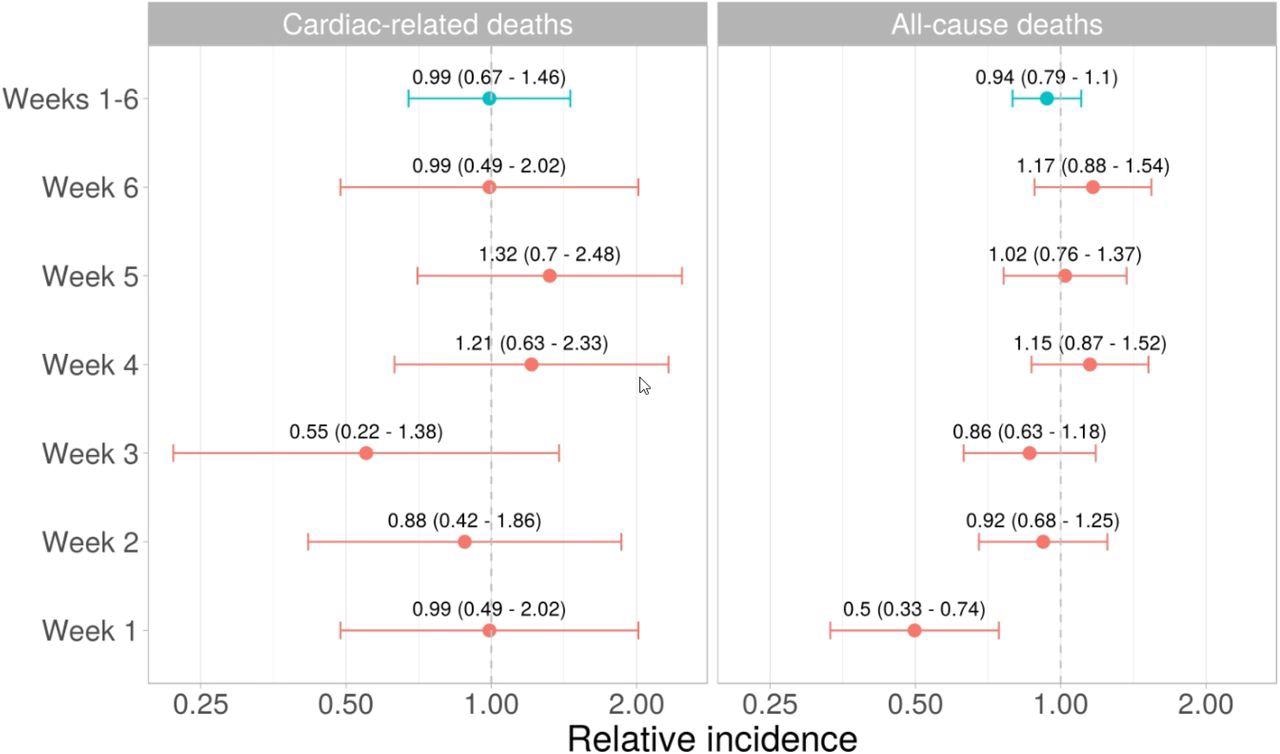 Relative incidence (95% confidence intervals) of cardiac death and all-cause death in the each of the 6 weeks in the risk period after the last vaccination received and in the risk period as a whole, compared to the baseline period.
Relative incidence (95% confidence intervals) of cardiac death and all-cause death in the each of the 6 weeks in the risk period after the last vaccination received and in the risk period as a whole, compared to the baseline period.
The analysis of death rates following SARS-CoV-2 testing revealed an increased risk of both cardiac and all-cause mortality following a positive test, with the greatest risk detected in the first week.
Conclusions
While COVID-19 has previously been linked to an increased risk of myocarditis and other cardiac events in young individuals, the current analysis reveals no evidence of an increased risk of death in the first 12 weeks after vaccination. While this finding is reassuring and should help combat vaccine hesitancy, many of the studies into adverse events following vaccination focus on specific vaccines, rather than vaccination alone.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Nafilyan, V., Bermingham, C., Ward, I. L., et al. (2022). Risk of death following SARS-CoV-2 infection or COVID-19 vaccination in young people in England: a self-controlled case series study. medRxiv. doi:10.1101/2022.03.22.22272775. hhttps://www.medrxiv.org/content/10.1101/2022.03.22.22272775v1
- Peer reviewed and published scientific report.
Nafilyan, Vahé, Charlotte R. Bermingham, Isobel L. Ward, Jasper Morgan, Francesco Zaccardi, Kamlesh Khunti, Julie Stanborough, Amitava Banerjee, and James C. Doidge. 2023. “Risk of Death Following COVID-19 Vaccination or Positive SARS-CoV-2 Test in Young People in England.” Nature Communications 14 (1): 1541. https://doi.org/10.1038/s41467-023-36494-0. https://www.nature.com/articles/s41467-023-36494-0.