In a recent study published in the journal Vaccines, researchers in Saudi Arabia and the United States examined immune responses and immunoglobulin G (IgG) cross-reactivity in individuals infected with Middle East respiratory syndrome coronavirus (MERS-CoV) and severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
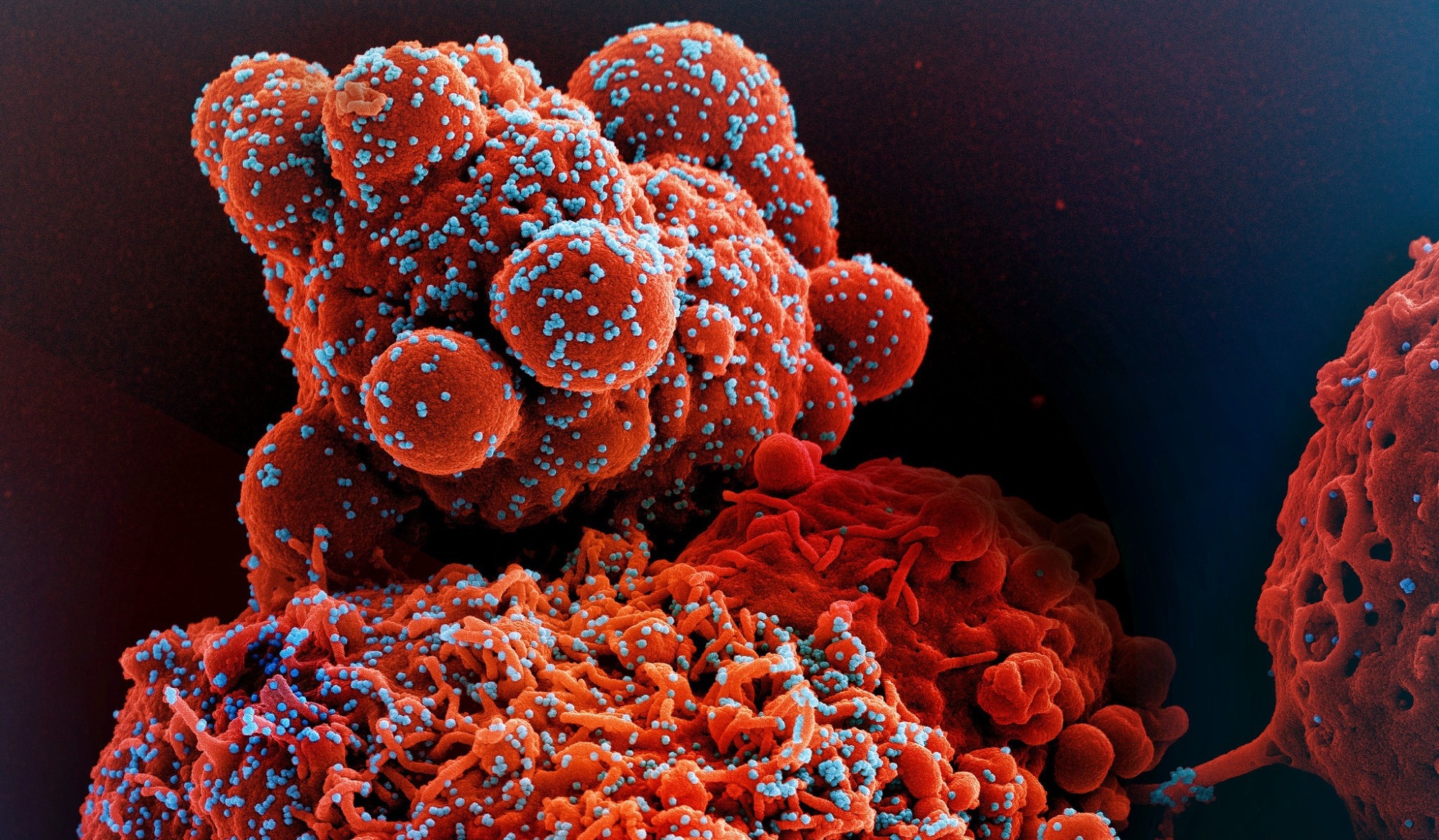 Image Credit: NIAID
Image Credit: NIAID
Human CoVs (HCoVs) are enveloped ribonucleic acid (RNA) viruses from the Coronaviridae family that cause influenza-like illness, pneumonia, bronchiolitis, and exacerbation of underlying lung disease. SARS-CoV-2, a novel beta CoV causing the coronavirus disease 2019 (COVID-19), was first detected in Wuhan, China, and has so far caused more than 757 million cases and 6.85 million deaths worldwide.
Another infectious respiratory disease, MERS, was first reported in 2012 in the Middle East. Globally, around 2,600 MERS-CoV cases have been recorded to date. MERS-CoV is endemic in the region and causes recurrent community outbreaks. Several SARS-CoV-2 variants have emerged throughout the COVID-19 pandemic. The impact of these variants on immunity against the virus may be influenced by previous exposure to related CoVs, such as MERS-CoV, SARS-CoV, and seasonal CoVs.
SARS-CoV, SARS-CoV-2, and MERS-CoV share a significant sequence homology and potential epitopes than can elicit adaptive immune responses. Moreover, a high level of cross-reactivity has been observed between B- and T-cell epitopes and antibodies against structural proteins of SARS-like viruses and SARS-CoV-2. Nonetheless, there is limited evidence on the cross-reactive immunity between MERS-CoV and SARS-CoV-2.
The study and findings
The present study evaluated humoral immune responses against SARS-CoV-2 and MERS-CoV in Saudi Arabian individuals. Eligible participants were 18 years or older and recruited into four groups – MERS-CoV/SARS-CoV-2 infection-naïve controls (C-Gp), SARS-CoV-2-infected individuals (SV-Gp), MERS-CoV-infected (MV-Gp) subjects, and MERS-CoV- and SARS-CoV-2-infected individuals (SV-MV-Gp).
Participants without a polymerase chain reaction (PCR) test and those with a known immunologic disease, malignancy, or on immunosuppressive therapy were excluded. Serum samples were collected and tested for antibodies against MERS-CoV and SARS-CoV-2 by enzyme-linked immunosorbent assay (ELISA). Specifically, IgG antibodies against the MERS-CoV S1 antigen and receptor-binding domain (RBD) of the SARS-CoV-1 spike were measured in the serum.
Thirty-four participants, including 12 females, with a mean age of 40.3, were recruited. Thirteen participants were controls; eight had SARS-CoV-2 infection, five had a history of infection with both viruses, and eight had MERS-CoV infection. Most participants (97%) received at least two doses of the COVID-19 vaccine.
All SV-MV-Gp and SV-Gp participants were double vaccinated, and three were boosted. Controls and individuals with SARS-CoV-2 infection alone showed no reactivity against MERS-CoV S1 antigen, whereas three MV-Gp and two SV-MV-Gp participants showed reactivity. Among SV-MV-Gp participants, 40% had positive borderline IgG reactivity against MERS-CoV compared to 37.5% of MV-Gp subjects. The IgG levels between MV-Gp and SV-MV-Gp subjects were statistically correlated.
Conclusions
In summary, the study showed that people with a history of SARS-CoV-2 and MERS-CoV infections exhibit significantly elevated IgG levels against MERS-CoV than those infected with MERS-CoV. The findings suggest that cross-reactive immune responses from common HCoVs can shape SARS-CoV-2 immunity. Notably, the sample size was small, warranting large-scale multicenter studies in the future.