New research reveals that what men eat, especially a Mediterranean diet or ultra-processed foods, can make a real difference to sperm quality and fertility potential.
 Role of Mediterranean Diet and Ultra-Processed Foods on Sperm Parameters: Data from a Cross-Sectional Study. Image Credit: Maly Designer / Shutterstock
Role of Mediterranean Diet and Ultra-Processed Foods on Sperm Parameters: Data from a Cross-Sectional Study. Image Credit: Maly Designer / Shutterstock
In a recent study published in the journal Nutrients, researchers in Italy evaluated the role of the Mediterranean diet (MD) and ultra-processed foods (UPFs) on sperm parameters.
Infertility is defined as the inability to achieve pregnancy after one year of regular, unprotected sex. It affects 15% to 25% of couples, or around 186 million individuals worldwide. Besides, male infertility is often multifactorial, involving genetic factors, lifestyle habits, environmental factors, and medical conditions. Lifestyle factors could negatively affect sperm parameters and overall reproductive health. Adherence to healthy diets, including MD, is associated with improved seminal parameters.
However, the associations between male fertility and UPFs are less well-defined. The optimal intake of minerals, vitamins, and antioxidants, particularly from food sources, plays a vital role in spermatogenesis. The MD adequately provides these oligo-nutrients. However, UPFs are industrially produced and contain ingredients not found in natural foods (e.g., additives, refined sugars). As such, UPFs lack essential vitamins, fiber, and minerals. UPFs also disproportionately derive calories from carbohydrates (mean 17.4% of total calories), compared to proteins (3.8%) or lipids (8.1%). Increasing literature also links UPF consumption to elevated risks of non-communicable diseases and cancer.
Importantly, while adherence to the MD has been linked to better semen parameters and reproductive capacity, high UPF intake may negatively affect sperm quality.
About the study and methods
In the present study, researchers examined the role of MD and UPFs on sperm parameters. Participants were males aged 18–60 attending an Italian Hospital for semen analysis between September 2022 and April 2024. Semen was collected three to seven days after sexual abstinence; semen pH and volume, sperm concentration, cell viability and morphology, and total sperm count were evaluated.
Further, plasma levels of luteinizing hormone (LH), follicle-stimulating hormone (FSH), sex-hormone-binding globulin (SHBG), and testosterone were measured. The MD Adherence Screener (MEDAS) questionnaire evaluated MD adherence. UPF intake was assessed using the 24-hour Food Recall Questionnaire. Analysis of variance (ANOVA) was performed to examine differences between continuous variables, whereas Fisher’s exact or chi-squared test was used for discrete variables.
Pearson’s correlation coefficient was used to evaluate correlations between variables. Further, multivariate analyses compared semen parameters strongly associated with UPF intake and MEDAS scores. Logistic regression was performed to assess the associations between ordinal and continuous variables and sperm count ≥ 39 million per ejaculate, and to estimate the corresponding odds ratios and 95% confidence intervals. The study also excluded individuals with conditions or behaviors known to affect fertility, such as those taking certain medications, those with chronic illnesses, or those engaging in high levels of physical activity (more than 3 hours per week).
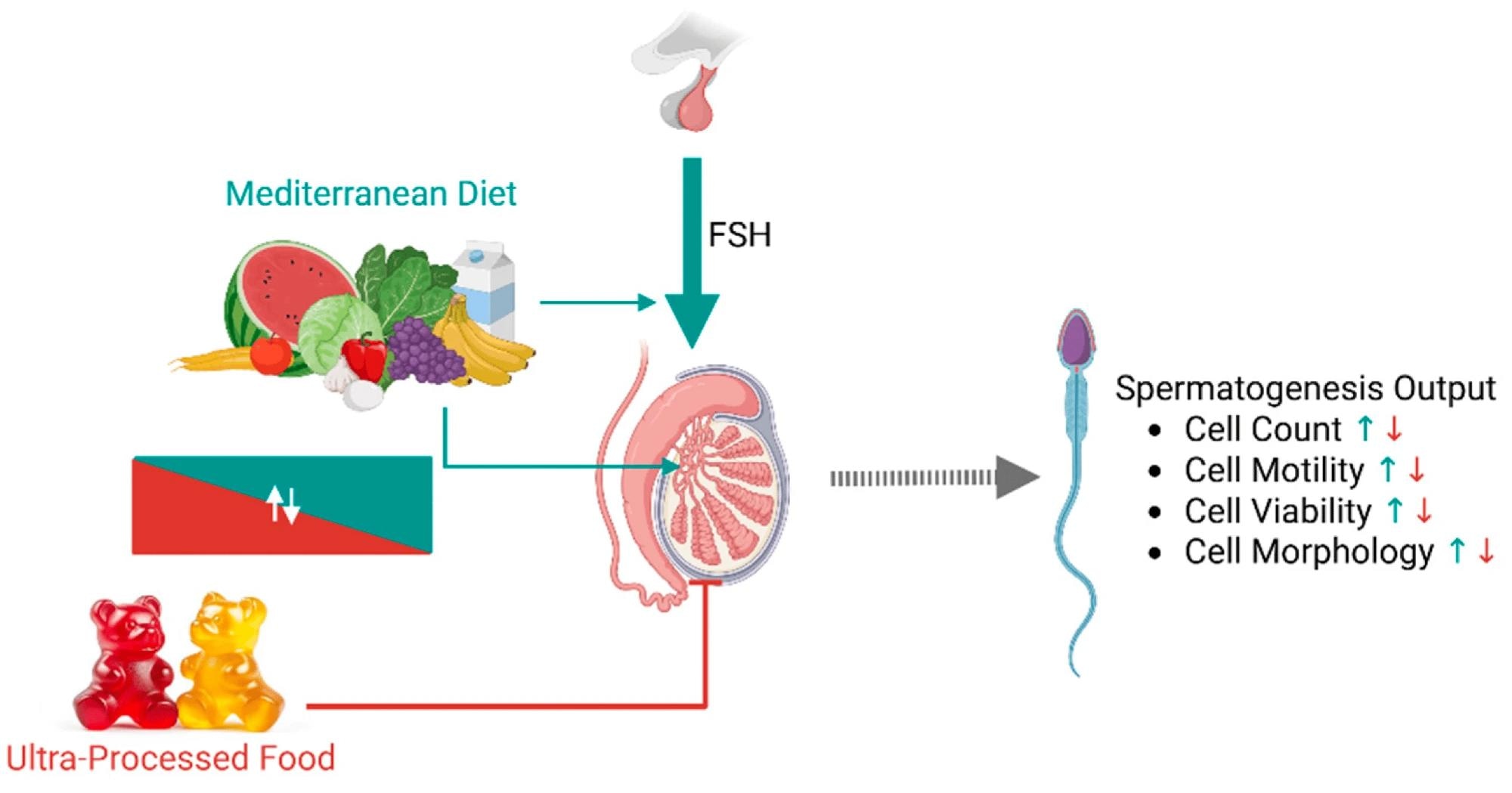 Representative scheme summarizing the possible mechanistic influences of dietary patterns on spermatogenesis. Adherence to the Mediterranean diet (MD) likely has a direct positive effect on the different cell populations of the seminiferous tubules due to its composition rich in polyunsaturated fatty acids and oligo-elements. In parallel, MD may positively influence the hypothalamic-pituitary-gonadal axis by enhancing testis sensitivity to follicle-stimulating hormone (FSH) or by reducing negative feedback at the central level. Ultra-processed food intake negatively influences testis function, both because it is inversely related to MD adherence and due to the reduced content of protective factors. Green and red arrows indicate, respectively, positive and negative effects.
Representative scheme summarizing the possible mechanistic influences of dietary patterns on spermatogenesis. Adherence to the Mediterranean diet (MD) likely has a direct positive effect on the different cell populations of the seminiferous tubules due to its composition rich in polyunsaturated fatty acids and oligo-elements. In parallel, MD may positively influence the hypothalamic-pituitary-gonadal axis by enhancing testis sensitivity to follicle-stimulating hormone (FSH) or by reducing negative feedback at the central level. Ultra-processed food intake negatively influences testis function, both because it is inversely related to MD adherence and due to the reduced content of protective factors. Green and red arrows indicate, respectively, positive and negative effects.
Findings
The study included 358 males, with a mean age of 34.6 and body mass index (BMI) of 24.4 kg/m². The mean MEDAS score of the sample suggested average MD adherence. MEDAS scores had a significant positive correlation with seminal parameters and a negative correlation with percentage of calories from UPFs (%Kal-UP) and serum LH and FSH levels.
Conversely, %Kal-UP was negatively correlated with all seminal parameters. The MEDAS score and %Kal-UP were not associated with BMI or age, and the correlations between MEDAS or %Kal-UP and semen parameters remained significant after controlling for BMI and age, indicating that these associations are independent of these confounders. Sperm parameters were significantly different across categories of MD adherence, with mean values of total sperm count, progressive motility, sperm viability, and sperm concentration increasing with MD adherence. Meanwhile, FSH levels were lower in individuals with moderate or high MD adherence compared to those with low adherence.
Testosterone and SHBG levels did not differ significantly across MD adherence categories. Since discrete categories of UPFs were unavailable, an unbiased stratification was performed by increasing quartiles of %Kal-UP (Q1–Q4). There was a significant decrease in mean values of total sperm count, sperm concentration, progressive motility, and percentage of sperm with typical morphology from Q1 to Q4.
Notably, individuals in the low MD adherence category and those in Q4 of %Kal-UP exhibited significantly lower values of sperm parameters compared to those in the high adherence category and Q1 of %Kal-UP. Furthermore, participants were stratified into two categories based on FSH levels: normal (<8 IU/mL) and high (>8 IU/mL) for the multivariate analysis.
Among participants with normal FSH levels, the mean values of total sperm count, sperm concentration, percentage of immotile cells, and percentage of progressive motile cells showed a significant decline with increasing quartiles of %Kal-UP. By contrast, individuals with high FSH levels showed no effects on these parameters by %Kal-UP quartiles.
A significant increase in total sperm count and concentration was noted with higher MD adherence, but only in individuals with normal FSH levels. Moderate and high MD adherence categories were associated with a significantly lower risk of low sperm count. On the other hand, Q3 and Q4 of %Kal-UP were associated with a significantly higher risk of total sperm count < 39 million per ejaculate. However, when high FSH levels (≥8 IU/mL, indicative of primary testicular impairment) were included in the analysis, FSH emerged as the dominant predictor of reduced sperm count, and dietary associations became less pronounced.
Study limitations
The authors note that the cross-sectional and observational nature of the study prevents any causal inference. Additionally, UPF intake was estimated from a single 24-hour recall, which can introduce error, and hormonal data were available only for a subset of participants. As a result, findings should be interpreted with caution and validated by further research.
Conclusions
In summary, the study demonstrated significant correlations between MD adherence and UPF intake and seminal parameters. The findings underscored an interplay between plasma FSH levels, MD adherence, UPF intake, and seminal parameters. With high FSH levels, reflecting primary testicular impairment, the dietary pattern had mild or null associations with seminal parameters.
Likewise, UPF intake had fewer associations with sperm parameters. In contrast, with normal FSH, suggestive of preserved testicular function, greater MD adherence was associated with a better seminal profile, while UPF intake showed an opposite association. These findings support the role of dietary interventions as potential modifiable risk factors for managing male infertility, particularly in men with preserved testicular function.
Journal reference:
- Petre GC, Francini-Pesenti F, De Toni L, et al. Role of Mediterranean Diet and Ultra-Processed Foods on Sperm Parameters: Data from a Cross-Sectional Study. Nutrients, 2025, DOI: 10.3390/nu17132066, https://www.mdpi.com/2072-6643/17/13/2066