Nine independent modeling teams demonstrate that maintaining a universal COVID-19 vaccine policy yields consistent population-level benefits, reducing hospitalizations and deaths beyond high-risk-only strategies, even as immune escape shifts the timing of seasonal peaks.

Study: Scenario Projections of COVID-19 Burden in the US, 2024-2025. Image Credit: Ground Picture / Shutterstock
In a recent study published in the journal JAMA Network Open, researchers projected United States (US) COVID-19 hospitalizations and deaths for April 2024-April 2025 under varying vaccination recommendations and immune escape assumptions, quantifying the benefits of each strategy.
Background
One season can still change thousands of lives: even in 2023-2024, COVID-19 killed more Americans per hospitalization than seasonal influenza. Decisions by the Advisory Committee on Immunization Practices (ACIP) guide the Centers for Disease Control and Prevention (CDC) in recommending who should be vaccinated; however, the evolution of variants and waning immunity keep the goalposts moving. Communities weigh convenience, cost, and fatigue against the need for protection for older adults and people with underlying health conditions. Families and hospitals plan for expected winter peaks, yet summer surges can still come as a surprise. Policymakers need numbers, not guesswork, to set broad or targeted guidance. Further research is required in order to compare realistic vaccination pathways amid immune escape.
About the study
The US Scenario Modeling Hub convened nine independent teams to produce projections of COVID-19 hospitalizations and deaths from April 28, 2024, to April 26, 2025. Teams calibrated models to weekly hospital admissions from the National Healthcare Safety Network (NHSN) and deaths from the National Center for Health Statistics (NCHS), using routinely collected, anonymized surveillance. Six scenarios crossed two axes: immune escape at 20% per year (low) or 50% per year (high) for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), and vaccine policy, 1) no recommendation (except for vaccine-naive children aging into eligibility at 6 months); 2) recommendation only for high-risk groups (adults ≥65 years or individuals with underlying conditions); or 3) recommendation for all persons aged ≥6 months.
Vaccines were reformulated to target circulating variants as of June 15, 2024, and were expected to be available as of September 1, 2024, with 75% vaccine effectiveness (VE) against hospitalization at release. State- and age-specific coverage was matched to observations from September 2023 to April 2024. Each team specified infection-acquired immunity and waning. Individual projections were combined via a trimmed linear opinion pool to form an ensemble; prevented burden under vaccination scenarios was estimated using meta-analytic methods. Uncertainty was summarized with 95% projection intervals (PI) and 95% confidence intervals (CI) where applicable.
Study results
Across all six scenarios, the models estimated that the U.S. COVID-19 burden from April 2024 to April 2025 would be similar to the prior year. Hospital admissions would remain below the CDC's “high” level overall, increasing from late summer into winter. In the worst case (high immune escape and no vaccine recommendation beyond baseline pediatric vaccinations), the projection was 931,000 hospitalizations (95% PI, 0.5-1.3 million) and 62,000 deaths (95% PI, 18,000-115,000) by April 26, 2025. In the best-case scenario (low immune escape, with vaccination recommended for everyone), the projection was 550,000 hospitalizations (95% PI, 296,000-832,000) and 42,000 deaths (95% PI, 13,000-72,000). Under assumptions most likely for 2023-2024 (high immune escape with a universal recommendation), projections were 814,000 hospitalizations (95% PI, 400,000-1.2 million) and 54,000 deaths (95% PI, 17,000-98,000). Adults aged ≥65 years accounted for 51%-62% of hospitalizations and 84%-87% of deaths.
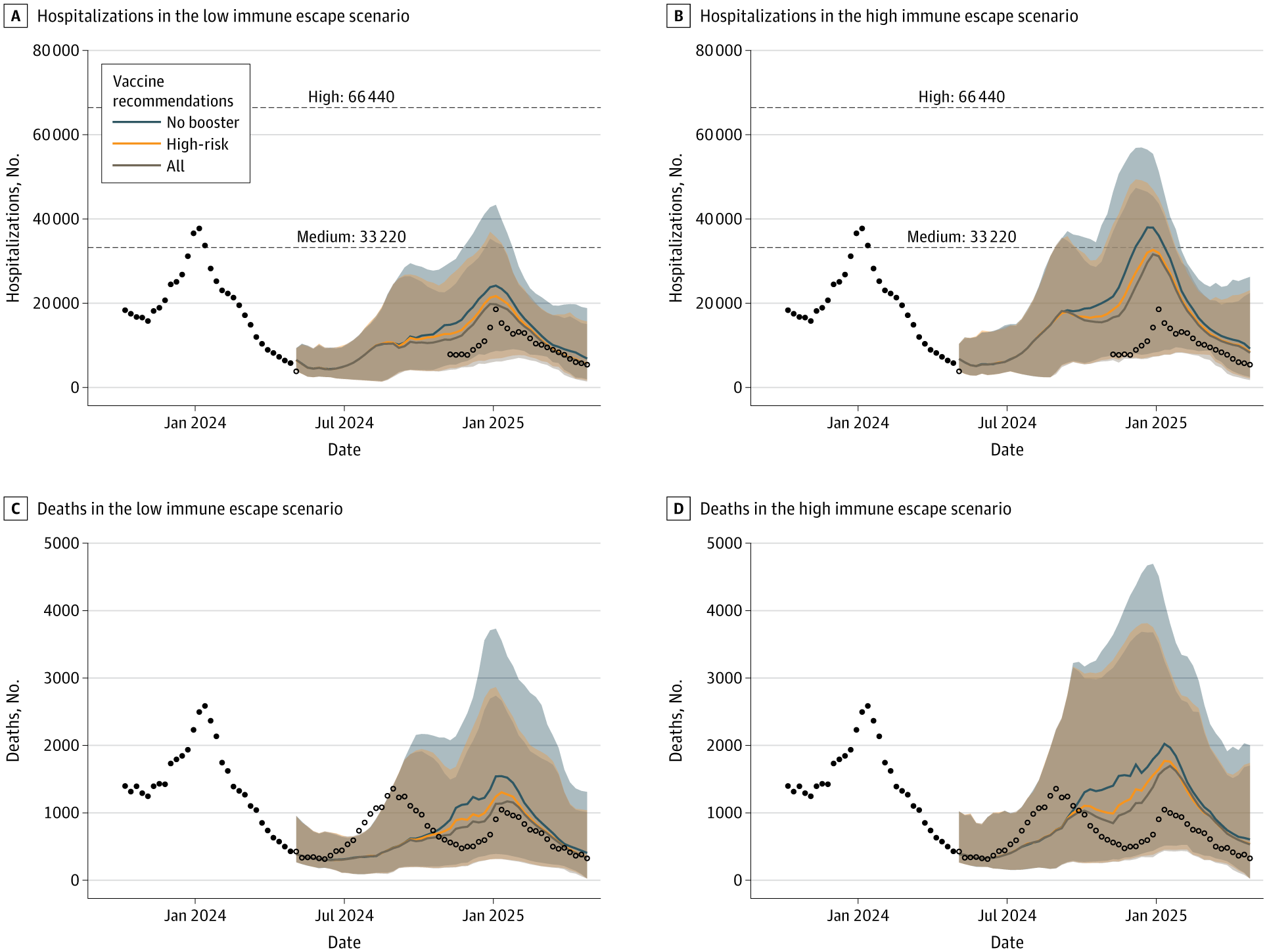
Weekly Projections of COVID-19 Hospitalizations and Deaths in the United States During April 28, 2024, to April 26, 2025, Across 6 Scenarios of Immune Escape and Vaccination Recommendations. Ensemble projections are based on 9 models, and historical data are shown as black points. Unfilled data points represent observed data after the projection period. National Healthcare Safety Network hospitalization data are shown only where the reporting fraction was greater than 75%, highlighting the gap in reliable data during this time (May 5, 2024, to November 2, 2024). Projection curves are colored based on vaccine recommendations, with curves representing the median of the ensemble projection and shading showing the 90% projection interval. Dashed lines indicate the Centers for Disease Control and Prevention thresholds for high and medium hospital admission levels (>20 and 10-20 weekly hospitalizations per 100,000, respectively).
Vaccination policies reduced the burden in both immune-escape regimes. Recommending vaccination only for high-risk groups reduced hospitalizations by 11% (95% CI, 6%-16%) under low immune escape and by 8% (95% CI, 5%-11%) under high immune escape; deaths fell by 13% (95% CI, 7%-18%) and 10% (95% CI, 6%-14%), respectively. Expanding to a universal recommendation yielded larger effects: hospitalizations fell by 15% (95% CI, 9%-21%) with low immune escape and 11% (95% CI, 7%-16%) with high immune escape, while deaths decreased by 16% (95% CI, 10%-23%) and 13% (95% CI, 8%-18%). In absolute terms, under high immune escape, vaccinating only high-risk groups averted 76,000 hospitalizations (95% CI, 34,000-118,000) and 7,000 deaths (95% CI, 3,000-11,000) versus no recommendation. Extending recommendations to all ages increased the impact to 104,000 hospitalizations (95% CI, 55,000-153,000) and 9,000 deaths (95% CI, 4,000-14,000) averted.
Compared with a high-risk-only policy, a universal policy provided additional indirect protection to older adults, preventing approximately 11,000 extra hospitalizations and approximately 1,000 extra deaths in those aged 65 years and older (representing a 3%-4% further reduction in burden for this group), reflecting community-level transmission benefits. Observed epidemiology diverged in timing from projections: the US experienced a notable summer 2024 wave peaking in August, followed by a smaller winter 2025 peak. This pattern aligns with higher effective immune escape in summer 2024 and lower in winter, differing from the model's assumption of constant annual escape. Despite timing discrepancies, ensemble coverage for weekly deaths was within expected ranges, and conclusions about the relative benefits of broader vaccination remained stable. The study noted limitations, including the potential for overestimating vaccine benefits if summer 2024 immunity exceeded projections.
Conclusions
To summarize, scenario-based modeling suggests that reformulated COVID-19 vaccination remains a viable tool to reduce hospitalizations and deaths in 2024-2025, particularly among adults aged 65 years and older and those with underlying conditions. While targeting high-risk groups alone yields substantial benefits, maintaining a universal recommendation offers additional, meaningful reductions, including indirect protection for older adults, under both low and high immune-escape conditions. Real-world variant dynamics may shift the timing of peaks, but the comparative advantages of broader vaccination persist. For households, clinics, and health systems planning the respiratory virus season, universal guidance can save thousands more lives than narrower strategies.
Journal reference:
- Loo, S. L., Jung, S.-M., Contamin, L., Howerton, E., Bents, S. J., Hochheiser, H., Runge, M. C., Smith, C. P., Carcelén, E. C., Yan, K., Lemaitre, J. C., Przykucki, E., McKee, C. D., Sato, K., Hill, A. L., Chinazzi, M., Davis, J. T., Bay, C., Vespignani, A., Chen, S., Paul, R., Janies, D., Thill, J.-C., Moore, S. M., Perkins, T. A., Srivastava, A., Al Aawar, M., Bi, K., Bandekar, S. R., Bouchnita, A., Fox, S. J., Meyers, L. A., Porebski, P., Venkatramanan, S., Lewis, B., Chen, J., Marathe, M., Ben-Nun, M., Turtle, J., Riley, P., Shea, K., Viboud, C., Lessler, J., & Truelove, S. (2025). Scenario Projections of COVID-19 Burden in the US, 2024-2025. JAMA Netw Open. 8(9). DOI:10.1001/jamanetworkopen.2025.32469 https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2839067