A major European review finds that childhood obesity prevention must begin before conception, addressing both parents’ health and the social systems shaping family behaviours.

Study: First 1000 Days Strategies to Prevent Childhood Obesity: A Narrative Review and Recommendations From the EndObesity Consortium. Image Credit: Pixel-Shot / Shutterstock
In a recent report published in the journal Pediatric Obesity, researchers from the European EndObesity Consortium synthesized evidence on the critical "first 1000 days," spanning preconception to 2 years. The consortium aimed to provide a novel narrative review identifying key risk factors and modifiable behaviours that might help mitigate the growing global burden of childhood obesity.
The report findings highlight that obesity-mitigating lifestyle interventions often start too late, overlook paternal factors, and fail to address social barriers inherent in several global cultural systems. These findings suggest that effective childhood obesity prevention requires a multi-pronged approach involving both parents, starting before conception, and supported by systemic policy changes.
Background
Childhood obesity is a significant global public health issue, characterized by substantial imbalances between a child’s calorie intake (e.g., overeating) and expenditure (e.g., sedentary lifestyle). The condition has previously been robustly associated with several chronic and life-threatening diseases including adult obesity, cardiovascular disease, and even premature death.
Alarmingly, statistics from the World Obesity Atlas 2024 estimate that over 750 million children aged 5–19 will be living with overweight or obesity by 2035, highlighting the need for urgent interventions to mitigate this silent global pandemic. Simultaneously, research leveraging large sample cohorts suggests that more than 60% of children with overweight or obesity remain living with overweight or obesity as adults.
Evidence increasingly suggests that most of the childhood obesity-associated risks are triggered in early life, during developmental adaptations to the environment in the womb and early childhood. While modifiable family lifestyle factors like diet, activity, and stress are known risks in childhood obesity incidence, most conventional prevention strategies have yielded disappointing results, with childhood prevalence continuing to rise despite global mitigation efforts.
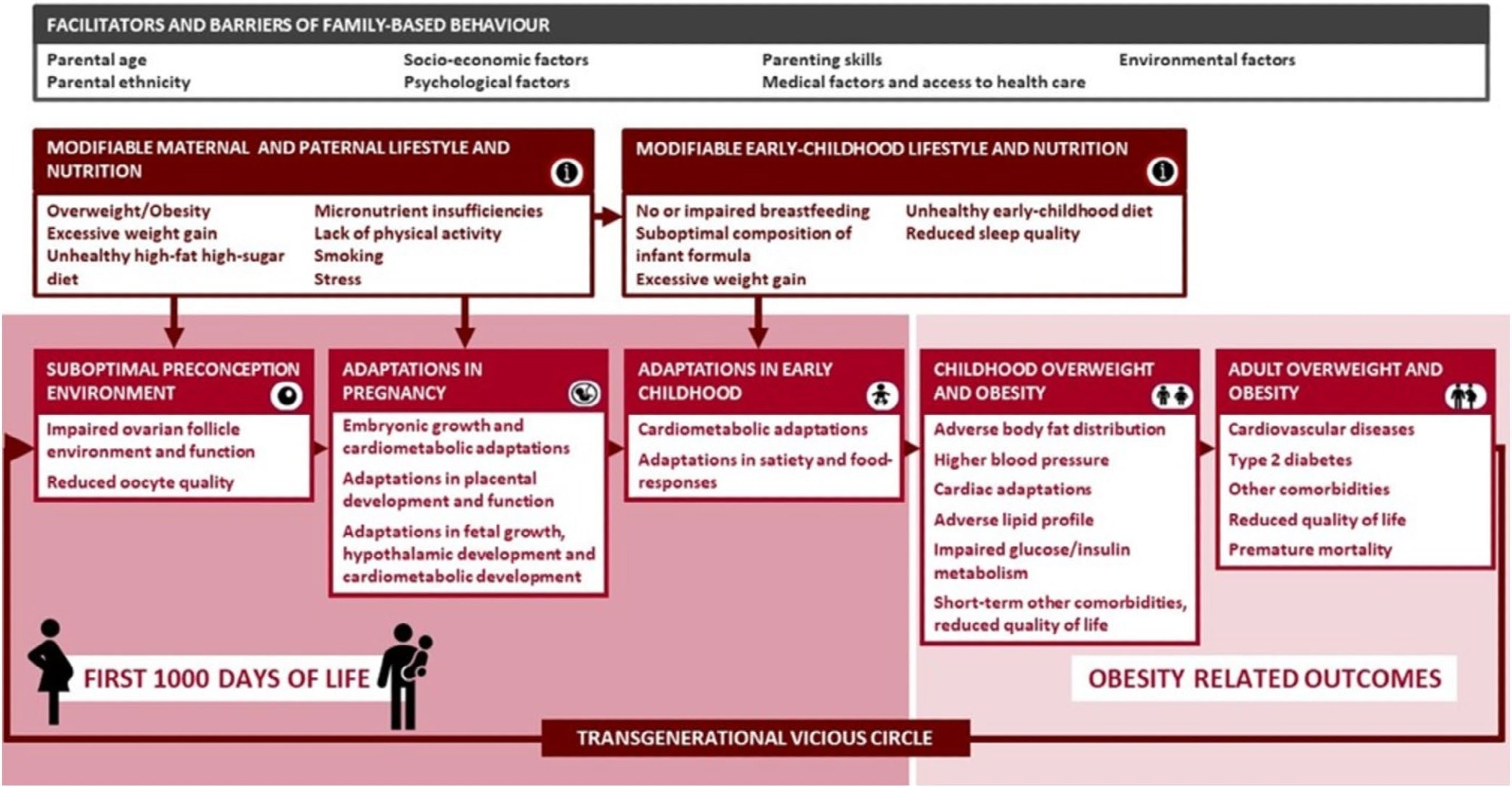
Conceptual framework for the EndObesity Consortium represents family-based adverse modifiable lifestyle factors in preconception, pregnancy and early-childhood related to increased risks of childhood obesity via independent effects and synergistic interacting effects. These factors urgently need to be used for prediction of childhood obesity and be the target of intervention strategies in these crucial transition periods. Maternal lifestyle and nutrition directly influence the preconception and pregnancy environment important for the oocyte and developing foetus. Paternal lifestyle influences maternal and family-based lifestyle, highlighting the importance of targeting both parents. Facilitators and barriers may influence these family-based health behaviours, behavioural change and obesity risk. These factors may also be used for prediction of childhood obesity and need to be considered in prevention and implementation strategies.
About the report
The present report supports childhood obesity mitigation efforts by summarizing the findings of the European Union’s (EU) EndObesity Consortium, a large-scale European collaboration funded by the EU’s Horizon 2020 program. The report is structured as a narrative review, synthesizing years of EndObesity Consortium data to identify gaps and build a new framework for prevention.
The review first analyzed observational and intervention data from 12 ongoing studies across Europe, conducted by six consortium partners, leveraging harmonized data from multiple large-scale birth cohorts. Subsequently, existing intervention studies were identified, screened for intervention/outcome relevance, and systematically reviewed to elucidate the benefits and limitations of conventional obesity-mitigating interventions.
Finally, the consortium (comprising researchers, stakeholders, parents, and representatives of public health organizations) compiled both long-term EndObesity Consortium data and systematic review outcomes to hold consensus discussions and develop evidence-based recommendations for research, clinical practice, and public policy.
Report findings
The EU consortium’s report reveals that current obesity prevention approaches suffer from three critical shortcomings: first, interventions focus too narrowly on pregnant mothers, largely ignoring paternal and preconception health.
Specifically, multi-cohort analyses revealed that paternal factors, such as BMI and diet, are independently associated with offspring obesity risk. Furthermore, very few families (between 1.9% and 3.7%) were observed to meet the criteria for an optimal "parental" healthy lifestyle score during pregnancy, with higher socioeconomic position associated with healthier parental lifestyle behaviours.
Second, the report highlights that in most cases, childhood obesity-mitigating interventions are often initiated too late. Notably, a scoping review of 20 prenatal lifestyle trials involving 11,385 women found no significant impact on weight, length, or body mass index (BMI) in their children (aged 1 month to 7 years), likely reflecting late initiation, short duration, small sample sizes, loss to follow-up, and limited process evaluation that reduced the power to detect effects.
Specifically, most lifestyle programs beginning in the second trimester or later were found to be too short to be effective. Conversely, interventions specifically tailored for socio-economically disadvantaged families were found to produce the most substantial population-wide benefits. The review further emphasizes co-creation with parents and multi-sectoral collaboration to improve intervention reach and sustainability.
Finally, among evaluated intervention trials, the clearest child-weight benefits were seen with infant-feeding strategies that reduced early protein intake and limited unmodified cow’s milk during infancy and toddlerhood. These strategies, including the use of lower-protein infant formulas when breastfeeding is not possible, show the most consistent evidence of benefit on child weight outcomes.
Conclusions
The present report by the EU’s EndObesity Consortium concludes that successfully addressing childhood obesity requires a fundamental strategy transition from simple dietary advice and preparation that begin well before conception. However, existing data is insufficient to accurately identify generalizable changes that would benefit global childhood obesity outcomes, necessitating future research (randomized controlled trials [RCTs]) that begin before conception and include both parents.
For clinicians, the report recommends using dynamic prediction tools to identify high-risk families early, noting that current models are often static and that EndObesity is developing dynamic models spanning preconception to infancy to better target prevention. The report also advises adopting sensitive, non-stigmatizing communication. Most importantly, the report calls for a policy shift toward “societal accountability.” This includes structural changes like food advertising restrictions and public health initiatives that make healthy choices accessible for all families, guided by proportionate universalism principles and multi-sectoral implementation frameworks, breaking the intergenerational cycle of obesity, especially prevalent in higher-income Western societies.
Journal reference:
- Schipper, M. C., Manshanden, A., Philippe, K., Ferré, N., Luque, V., Lecorguillé, M., Aubert, A. M., Guerlich, K., Le Gal, C., Feher, S., Parada‐Ricart, E., Escribano, J., Grote, V., Koletzko, B., Primavesi‐Poggio, T., Reiss, K., Seidell, J. C., Lioret, S., Phillips, C. M., … Gaillard, R. (2025). First 1000 Days Strategies to Prevent Childhood Obesity: A Narrative Review and Recommendations From the EndObesity Consortium. Pediatric Obesity. DOI: 10.1111/ijpo.70060. https://onlinelibrary.wiley.com/doi/10.1111/ijpo.70060