A major retrospective study shows that people with blood group A face a higher likelihood of autoimmune liver disease, especially primary biliary cholangitis, while those with blood group B appear less vulnerable.
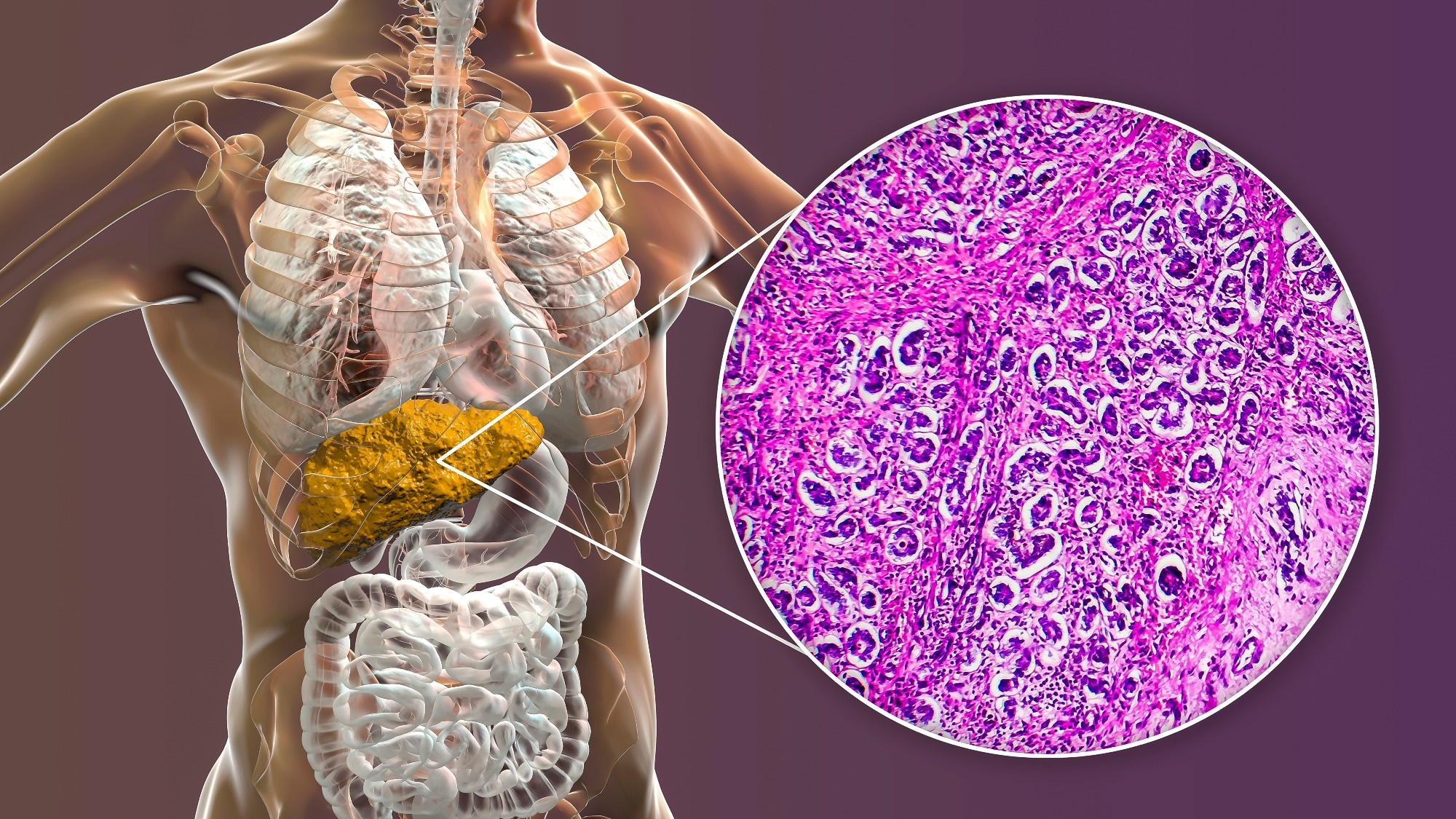 Study: Association between ABO blood group system and autoimmune liver disease. Image credit: Kateryna Kon/Shutterstock.com
Study: Association between ABO blood group system and autoimmune liver disease. Image credit: Kateryna Kon/Shutterstock.com
Individuals who have blood group A may be at higher risk of developing autoimmune liver disease, particularly primary biliary cholangitis (PBC). At the same time, no significant association was observed for autoimmune hepatitis (AIH), as reported by a new study published in Frontiers in Medicine.
What the ABO system means
The ABO blood group system in humans is based on the expression of A, B, or H antigens of carbohydrate epitopes on the surface of red blood cells (RBCs) and glycolipids. The system comprises four blood groups: A, B, AB, and O. A vast body of evidence suggests that the ABO blood group is associated with various diseases, including cancer, vascular diseases, gastroduodenal ulcers, severe Plasmodium falciparum malaria, and diabetes.
A few studies have linked the ABO blood group with autoimmune disease risk. However, the results remain inconsistent. Among patients with rheumatoid arthritis, a more frequent distribution of A and Rh-positive blood groups has been reported. These findings suggest a possible interference between the pathway of blood group production and auto-antibodies.
Autoimmune liver disease is a chronic condition in which the body’s immune system mistakenly attacks the liver, resulting in inflammation and damage. Autoimmune hepatitis, primary biliary cholangitis, and primary sclerosing cholangitis are major forms of autoimmune liver disease.
Both genetic and environmental factors, as well as their cross-interactions, significantly contribute to the pathogenesis of autoimmune liver disease. Individuals with a genetic susceptibility may produce abnormal immune responses in response to environmental factors, leading to autoimmune-mediated liver cell damage.
Given the association between ABO blood group and autoimmune antibody production, there remains a possibility that ABO blood group may also affect the pathogenesis of autoimmune liver disease.
In the current study, researchers from Tangdu Hospital and Xi'an Gaoxin Hospital, China, investigated the relationship between ABO blood group and the incidence of autoimmune liver disease. Their primary goal was to provide clinical evidence to enhance disease diagnosis and treatment.
Key patterns identified
The study included a total of 114 patients with autoimmune liver disease and 1,167 healthy individuals (controls). Among 114 patients, 44 were diagnosed with autoimmune hepatitis, and 70 were diagnosed with primary biliary cholangitis.
The analysis of ABO blood group distribution revealed that blood group A is the most prevalent one among patients with autoimmune hepatitis and primary biliary cholangitis, followed by blood groups O, B, and AB.
Compared to healthy controls, ABO blood groups exhibited a significant difference in distribution among patients with primary biliary cholangitis, but not among patients with autoimmune hepatitis.
Specifically, the findings revealed that individuals with blood group A have a significantly higher risk of developing primary biliary cholangitis. In contrast, those with blood group B are significantly less susceptible to developing the disease.
Further statistical analysis revealed that blood group A is significantly more prevalent and blood group B is significantly less prevalent among patients with autoimmune liver disease. However, no significant difference was observed for the other two blood groups. PBC primarily drove these associations, as AIH showed no statistically significant differences compared to controls.
Implications for disease risk
The study highlights a link between ABO blood group distribution and the presence of autoimmune liver disease. Specifically, the study reports that blood group A is associated with a higher likelihood of primary biliary cholangitis.
Apart from playing a role in blood transfusion and blood typing, blood group antigens serve as cell surface receptors for various signaling molecules, and are involved in various physiological and pathological processes, including cell recognition, adhesion, intercellular signal transduction, immune response, inflammation, autoimmune diseases, aging, cancer cell growth and metastasis, and pathogen infection.
It is well documented in the literature that human leukocyte antigen (HLA) class I and II genes are strongly associated with the pathogenesis of autoimmune liver disease. In the immune system, these genes play a crucial role in distinguishing the body’s own cells from foreign invaders, such as pathogens and cancer cells.
The link between blood group A and the incidence of autoimmune liver disease identified in this study may be explained by the fact that individuals with this blood group carry multiple high-risk HLA alleles, which are known to increase the risk of developing autoimmune liver disease. However, these mechanisms are hypothetical and were not directly tested in the study.
Existing evidence also indicates that the HLA-DRβ chain shares structural similarity with blood group A antigen. This similarity may lead to activation of B cells targeting blood group A antigens, subsequently inducing the production of cross-reactive autoantibodies that attack liver cells.
ABO blood group antigens are widely expressed in the intestine and thus can indirectly regulate immune functions by shaping microbiota colonization. In individuals with blood group A, the A antigen can act as an adhesion receptor for symbiotic bacteria, resulting in the enrichment of specific bacterial communities. These bacterial communities can induce T helper cell differentiation, increase inflammation, and trigger immune infiltration in the liver.
Overall, the study findings support the inclusion of ABO blood group analysis in clinical settings to identify individuals who are at higher risk of developing autoimmune liver disease, particularly primary biliary cholangitis.
Download your PDF copy now!