The pandemic of COVID-19 that is circulating the world, causing casualties by the hundreds of thousands, and millions of admissions, is the result of infection by the novel coronavirus severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The infection is mostly asymptomatic but can cause pneumonia and acute respiratory distress syndrome (ARDS) in a significant minority of patients.
COVID-19 and Clots
The most common cause of death is ARDS; however, organs other than the lungs are also severely affected, as seen with acute cardiac injury and acute kidney failure. A high level of inflammation is also present in patients with severe illness, as evidenced by high D-dimer levels and procoagulant changes that predispose to intravascular clot formation. Accordingly, both arterial and venous clotting events have been reported in these patients.
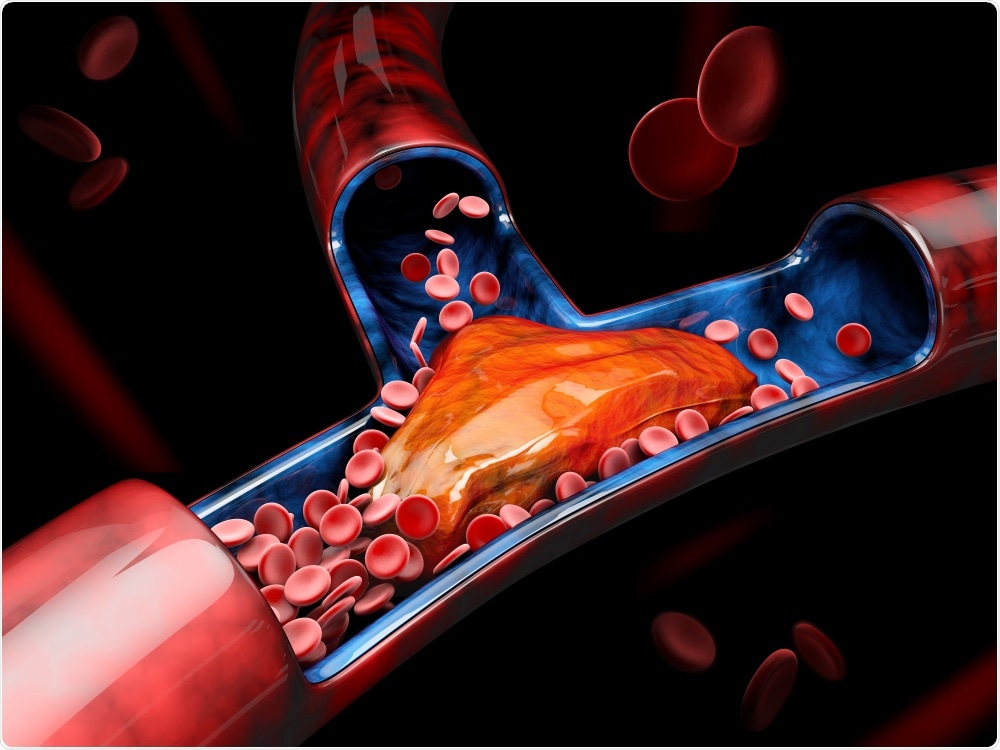
Study: Venous Thrombosis Among Critically Ill Patients With Coronavirus Disease 2019 (COVID-19). Image Credit: Victor Josan / Shutterstock
Deep Vein Thrombosis – Complications
Deep vein thrombosis (DVT) can have a number of serious sequela. For instance, the clot may be dislodged from the vein and travel through the circulation back to the heart and into the lungs to cause a pulmonary embolism (PE).
PE causes a block in the arteries of the lung, causing acute shortness of breath, chest pain on breathing in, and coughing up blood. The patient may go into shock, suffer right ventricular failure, or die, in some cases.
Survivors may suffer from pulmonary hypertension. Other more chronic consequences are venous insufficiency and post-thrombotic syndrome.
Deep Vein Thrombosis – Causes
The reasons for an increased frequency in critically ill patients include their immobility, the vascular injury caused by frequent blood tests and indwelling catheters, renal problems, and the triggering of inflammatory and coagulation cascades. Earlier studies have shown that venous thromboembolism occurs in up to 10% of critically ill patients even when they are on adequate anticoagulation therapy.
How the Study Was Done
The current study was motivated by the reports of increased levels of inflammatory markers, early reports that deep vein thrombosis was more frequent in seriously ill COVID-19 cases, and increased rates of this complication in the first few patients with COVID-19 at the researchers’ hospital.
The study was performed at an intensive care unit in France, in a suburb of Paris, from the middle of March 2020 to the beginning of April 2020. There were 34 patients, all diagnosed to have ARDS. Nasopharyngeal swabs from 26/34 patients had a positive reverse-transcriptase polymerase chain reaction (RT-PCR), while 8 were negative on PCR but showed the typical signs of COVID-19 pneumonia on chest CT scan.
The patients in the study were aged 62 years, on average, and the majority (25/34, or 78%) were men. The most common co-existing illnesses were diabetes (15/34, or 44%), diabetes (13/34, or 38%), and obesity (mean body mass index, BMI, 31.4).
A routine venous ultrasound examination was performed at the time of admission, and those patients with negative findings, it was repeated after 48 hours.
What the Study Showed
Of the 34 patients, 22, or 65%, had deep vein thrombosis at the time of admission, and in another 5 patients, bringing the total up to 27 (79%), at the time of repeat venous ultrasound. In 18 of the patients or over 50%, bilateral deep vein clots were found to be present. In a quarter of patients (9/34), the clot was within the veins nearer the heart.
The mean D-dimer level in this population was 5.1 μg/mL, with a fibrinogen level of 760 mg/dL, and C-reactive protein 22.8 mg/dL.
Among the 15 patients with diabetes in total, for instance, 12 developed deep vein thrombosis. Similarly, for the 13 patients with hypertension, 9 developed thrombosis. The mean BMI was significantly higher, at 32.2, in the group that developed this complication compared to 27.8 in the other group.
The laboratory findings showed a higher white cell count, lymphocyte count, and platelet count in peripheral blood in the patients who developed deep vein thrombosis compared to the other group.
Importance of the Study
It is known that about half the patients with COVID-19 who develop critical illness will die. Anywhere from 27% to 69% of them will have venous thromboembolic events. Almost a quarter will have blood clots in the lungs.
The study is limited by the small size and the fact that it was carried out at a single center. However, since almost 80% of the patients developed deep vein thrombosis, it is reasonable to suspect that early screening for and treatment of this complication would contribute lowering the high mortality rate.
Moreover, the usefulness of instituting routine anticoagulant prophylaxis for all critically ill COVID-19 patients should also be considered, since one in seven patients in the current study had deep vein thrombosis even while they were on such a regimen.
Journal reference:
- Nahum J, Morichau-Beauchant T, Daviaud F, et al. Venous Thrombosis Among Critically Ill Patients With Coronavirus Disease 2019 (COVID-19). JAMA Netw Open. 2020;3(5):e2010478. doi:10.1001/jamanetworkopen.2020.10478