Common blood test results may offer an early clue to bone loss, suggesting that alkaline phosphatase levels could help identify people who may benefit from earlier osteoporosis assessment before fractures occur.
Study: The relationship between serum total alkaline phosphatase and risk of osteoporosis: a cross-sectional study. Image Credit: Javier Regueiro / Shutterstock
In a recent study published in the journal Frontiers in Endocrinology, researchers investigated whether the routinely measured blood enzyme alkaline phosphatase (ALP) can serve as a marker for osteoporosis.
They found that higher ALP levels were consistently linked to a greater likelihood of osteoporosis, with stronger associations observed among metabolically healthy, younger, and female individuals, and identified a potential threshold for recommending further bone health assessments.
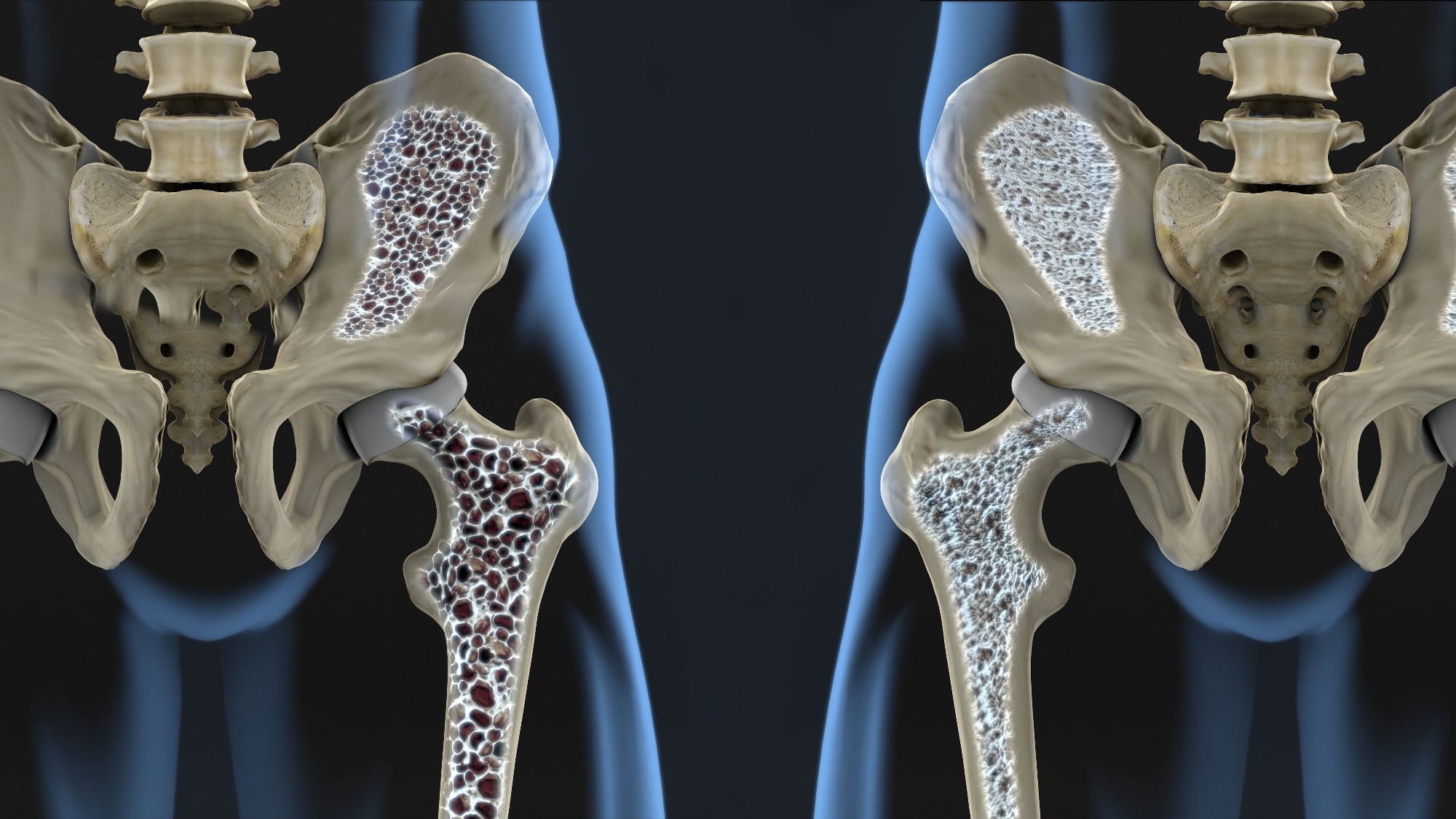
Osteoporosis Burden and Need for Accessible Biomarkers
Osteoporosis is characterized by reduced bone mass and structural deterioration, leading to an increased risk of fractures and substantial impacts on health and quality of life. As life expectancies increase, its prevalence is rising globally. As fracture incidence sharply increases with age, especially after 75, there is growing interest in identifying accessible biomarkers that can help detect bone loss earlier.
ALP, produced primarily by bone-forming osteoblasts and hepatocytes, plays a key role in bone mineralization by degrading pyrophosphate. Approximately half of ALP in the blood originates from bone, and bone-specific ALP closely tracks with total ALP levels in healthy and osteoporotic populations.
Total ALP is cheap and widely available in routine health checks, and researchers have explored its potential as a surrogate marker of bone health. However, previous findings are inconsistent, with some studies reporting negative associations between ALP and bone mineral density, and others finding no clear pattern.
Factors such as sample size, population heterogeneity, reliance on self-reported data, and metabolic or liver conditions that influence ALP further complicate interpretation.
Study Population and Clinical Assessments
Researchers aimed to clarify whether total ALP can reliably indicate osteoporosis risk in a large, systematically assessed population. They conducted their analysis using cross-sectional data from routine health examination records from a large teaching hospital in Chongqing, China, spanning 2019–2024.
Eligible participants were adults aged 20 or older who had completed blood ALP testing and dual-energy X-ray absorptiometry (DXA) scans of the hip and spine. Records with incomplete information were excluded, and when duplicate entries existed, only the most recent examination was considered.
Osteoporosis was diagnosed according to the World Health Organization (WHO) criteria using DXA T-scores, with modified definitions applied to younger adults. Standardized hospital procedures were used to collect anthropometric measurements, blood pressure, liver ultrasound findings, and biochemical markers, including glucose, lipids, uric acid, and liver enzymes. Definitions of metabolic abnormalities followed established medical guidelines.
Statistical analyses included descriptive comparisons, t-tests, chi-square tests, and five logistic regression models progressively adjusting for age, sex, body composition, metabolic markers, and liver function. Restricted cubic spline regression tested for non-linear associations between osteoporosis and ALP, while receiver operating characteristic (ROC) analysis assessed ALP’s predictive performance and identified an optimal cut-off value using Youden’s index.
Participant Characteristics and Initial Associations
Among 12,835 participants, 9.5% were diagnosed with osteoporosis, and nearly all individuals (99%) had ALP levels within the clinical reference range. Participants with osteoporosis had significantly raised ALP levels. Older individuals, females, and those with lower body weight or higher waist–hip ratios were more likely to have osteoporosis. Those at higher risk also showed higher systolic blood pressure, fasting glucose, total cholesterol, and high-density lipoprotein (HDL) levels, while uric acid and liver enzymes were lower. No differences were observed in diastolic blood pressure, triglycerides, or low-density lipoprotein (LDL).
ALP–Osteoporosis Associations Across Statistical Models
Logistic regression consistently demonstrated that each 1 IU/L increase in ALP was associated with higher odds of osteoporosis, with per-unit effect sizes modest but cumulative across the ALP range, and this association remained strong across all adjusted models. Spline analysis showed a mostly linear relationship, but the association flattened when ALP exceeded 100 IU/L. ROC analysis indicated poor-to-modest discrimination, with 72 IU/L emerging as the best cut-off for predicting osteoporosis.
Subgroup Differences and Metabolic Influences
Subgroup analyses revealed stronger statistical associations, rather than higher absolute risk, in women, younger individuals, and those with normal liver enzymes and healthier metabolic profiles. When liver enzymes were elevated, or when glucose or lipid profiles were abnormal, the association weakened substantially or disappeared, suggesting that metabolic and hepatic factors may distort the link between bone status and ALP.
Interpretation, Limitations, and Clinical Implications
This study found that higher serum total ALP is consistently associated with a greater likelihood of osteoporosis, even within the normal reference range and after adjusting for extensive confounders.
The association was strongest in younger women and metabolically healthy individuals, likely because ALP more accurately reflects bone-derived ALP when liver function and metabolic status are normal. Elevated ALP may represent a compensatory increase in bone turnover in response to declining bone density, rather than a direct cause of bone loss. However, when liver injury or metabolic abnormalities are present, the liver-derived component of ALP may dilute this relationship.
Strengths include the large sample, standardized clinical data, and detailed subgroup analyses. However, the study relied on a cross-sectional design, drew its population from a single center, and did not include information on physical activity, thyroid status, medication use, and diet, which limits the findings.
Overall, an ALP level around 72 IU/L may serve as a tentative threshold for recommending further assessments of bone health, though longitudinal cohort studies are required to confirm its causal and predictive value.