Recent advances in immuno-oncology have opened previously unimaginable avenues to produce cancer vaccines. An increasing amount of research shows that immunotherapy could be a powerful weapon in the fight against cancer.

Image Credit: PhotobyTawat/Shutterstock.com
Compared to traditional treatment methods that include surgery, chemotherapy, and/or radiotherapy, immunotherapy targets cancer cells more specifically, thus improving response rates and the quality of life of the patients.
Cancer vaccines can be used to target tumor-associated antigens, tumor-specific antigens, cancer germline antigens, or virus-associated antigens. Cancer vaccines could be peptide/protein-based, cell-based, or DNA/RNA (gene)-based, with different types of adjuvants.
By targeting specific antigens and private epitopes, the latest cancer vaccines could even have the potential to cure the disease. Personalized immunotherapies based on neoantigens are also being developed and are believed to be very effective in controlling tumor behavior.
A better understanding of the activation and function of T cells has paved the way for advances in cancer vaccine technology. Several types of platforms are being worked on for cancer therapy including virus vector vaccines, cellular vaccines, peptide vaccines, and molecular vaccines using DNA or RNA.
All these platforms are in the developmental stage and have their advantages and disadvantages.
DNA and RNA vaccines
The advantage of DNA and RNA vaccines is they are comparatively easy and produced at a lower cost. Therapeutic DNA vaccines may be a promising option to activate the immune system’s fight against cancer.
Though plasmid DNA vaccines had a good safety profile and generated a specific and broad immune response in clinical trials in the past, their therapeutic effects were modest because of the tumor’s immunosuppressive mechanisms.
DNA vaccines could successfully increase the immunogenicity by choosing the best antigen(s) to insert into the plasmid DNA. Another strategy involves combining DNA vaccines with other therapies that help attenuate immunosuppression by the tumor or increase the number or activity of immune cells.
RNA fares are better than DNA in cancer vaccines. While RNA is more prone to degradation than DNA, this can be minimized by chemical modifications and the addition of modified nucleosides like pseudouridine. RNA, unlike DNA, cannot integrate into the genetic code and hence has zero oncogenic potential.
Moreover, RNA has to enter only the cytoplasm, but DNA needs to go through an additional barrier - the nuclear membrane – into the nucleus.
Cellular vaccines
Vaccines that use either killed cancer cells or autologous antigen-presenting cells having cancer antigens have yielded some level of efficacy in patients. Both autologous tumor cells and irradiated allogeneic cells from tumor cell lines were tested in preclinical and clinical experiments.
Though such vaccines were successful in murine tumor models, many clinical trials using GVAX vaccines in melanoma, prostate cancer, lung cancer, and pancreatic cancer have shown only limited efficacy despite generating immune responses in the cancer patients.
Peptide vaccines
Single antigen-based short peptides are commonly used in vaccine clinical trials. Short peptides that have less than 15 amino acids do not require much processing by APCs and are capable of effectively binding to MHC class I molecules present on the surface of nucleated cells.
Work is ongoing to improve the quality and potency of peptide vaccines by fusing peptides with Toll-like receptor (TLR) agonists, adding powerful inflammatory adjuvants to peptides, and combining them with other immune modulators.
Viral vector vaccines
Many viruses have been tested as platforms for cancer vaccines. As human immune systems have evolved to respond promptly to viruses, virus-based vaccines can generate a strong and long-term response.
Viral vectors from adenoviruses, poxviruses, and alphaviruses are the most commonly used. One disadvantage of viral vector vaccines is that the antiviral response deactivates the vector and limits repeated vaccination.
What the future holds?
While the results of cancer vaccine trials have been encouraging so far, there are still some obstacles that we need to overcome. Cold tumors such as pancreatic and colorectal cancers have low response rates to cancer immunotherapies.
The ability of personalized cancer vaccines to increase the number of reactive T cells and thus response rates in cold tumors needs to be studied further.
Heterogeneity of tumors and immune escape are other concerns. The same neoantigens in a patient may be expressed only on some tumor cells but not others, which help some cells to escape immunotherapy. Some studies show that cancer vaccines that target multiple neoantigens may solve this problem to an extent by minimizing the chance of tumor escape.
Pharmacoeconomics is also crucial while considering the implementation of personalized neoantigen cancer vaccine into routine clinical practice. Individualized vaccines are still very expensive due to the high cost of genome sequencing and personalized drug manufacturing.
Automation and optimization of manufacturing methods and the development of better ways for prediction of antigen presentation will hopefully help improve the commercialization of personalized vaccines in the future.
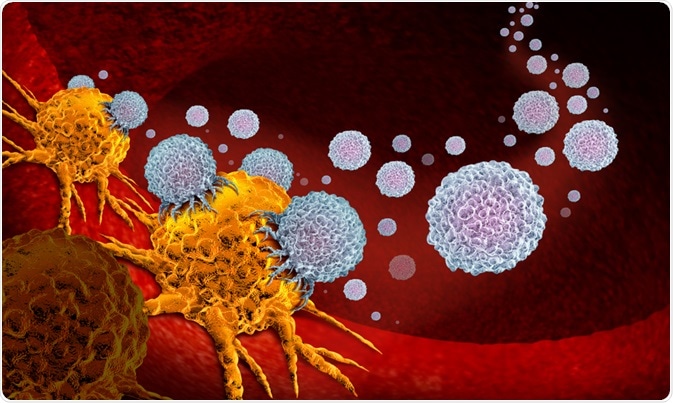
Image Credit: Lightspring/Shutterstock.com
Sources
Further Reading
Last Updated: May 21, 2020