Feb 8 2019
How bariatric surgery helps people with obesity and diabetes is related to changes in the way the gut senses food and nutrients after the operation, researchers report February 5 in the journal Cell Reports. They found that following surgery, altered patterns of digestion and absorption lower in the gut trigger production of higher levels of gut hormones, especially glucagon-like peptide 1 (GLP-1), which in turn causes higher insulin production.
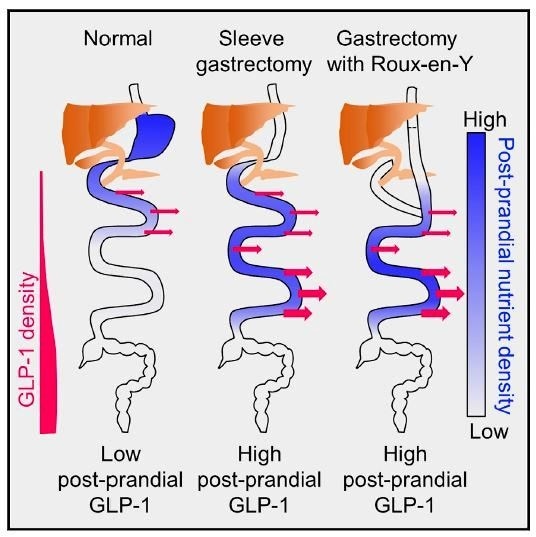
This graphical abstract shows that higher gut hormone levels after bariatric surgery are due to altered flow of nutrients that stimulates more distal enteroendocrine cells. Credit: Larraufie et al. - Cell Reports
"For people who have gastric bypass surgery to treat obesity and who also have diabetes, after surgery body weight is reduced and the diabetes melts away quickly," says senior author Fiona Gribble of the Cambridge University Metabolic Research Laboratories at the Wellcome Trust - MRC Institute of Metabolic Science. "But in lean patients with gastric cancer, they start off having normal glucose control and after the operation they end up having frequent hypoglycemic episodes because their sugar levels dip." The team wanted to learn more about the mechanism explaining these opposite results regarding glucose management.
Researchers have long known that bariatric surgery changes how the food you eat is digested and absorbed down the gut. They also knew that hormone-producing cells in the gut, such as GLP-1 and peptide-YY (PYY) are elevated afterwards. But they did not know the precise connection between these facts. For this study, the team decided to focus on GLP-1 as it is a major hormone involved in diabetes treatment. At least a half dozen GLP-1-based medications are available for managing Type 2 diabetes. "Our theory was that the high GLP-1 levels produced after surgery are quite important for improving your blood glucose after surgery," says Gribble.
The team studied five individuals receiving bariatric surgery for a hereditary form of gastric cancer. Participants received Exendin-9, a compound that blocks the action of GLP-1, at the same time as taking glucose by mouth. They found that concentrations of insulin, the hormone responsible for lowering blood glucose levels, did not increase as dramatically when these individuals were given Exendin-9 and did not suffer hypoglycemic episodes. "We found that blocking the GLP-1 hormone with the Exendin-9 blocked its effect on the pancreatic beta cells that produce the insulin," says Gribble.
The team also wanted to know why GLP-1 levels rise so high after surgery. Normally, food is digested and absorbed high up in the gut. But after surgery, it happens lower down because of the gut rearrangement that involves a Y-shape connection between the bile and pancreatic enzymes with the food. "Most digestion does not happen until the bile and the pancreatic enzymes coming down from one side join the food coming down the other side, which occurs lower in the gut," explains Gribble. That is important because most GLP-1 is released lower down the gut. "If you digest and absorb your nutrients a bit lower down, you consequently stimulate the release of much more GLP-1."
Using new RNA sequencing and mass spectrometry-based measurements they developed for this research, the team mapped the location of various hormonal peptides in the gut in humans and mice before and after surgery. They found that the cells producing the GLP-1 hormone and other gut hormones are not affected by the surgery. "This means that the reason for higher GLP-1 secretion is not because the surgery changes the hormone production by the gut, but it is because nutrient digestion and absorption happens in a different place in the gut and that causes higher levels of GLP-1 and PYY," says Gribble.
Looking forward, the team hopes to learn the precise mechanism responsible for the rapid weight loss in bariatric surgery. "If you can work that out and make a therapy that mimics that, that is what everyone wants: an injectable or oral medication that could mimic the surgery and cause weight loss in people without the surgery," she says. And for those suffering from hypoglycemia after gastric cancer surgery, development of a compound that blocks GLP-1 on a more permanent basis may help improve quality of life for patients who currently make significant adaptations to their eating behavior to avoid hypoglycemic episodes.