New evidence shows that human M cells act as fully fledged antigen-presenting cells, processing and presenting gluten peptides through a dendritic cell-like pathway that may shape early coeliac disease immunity.
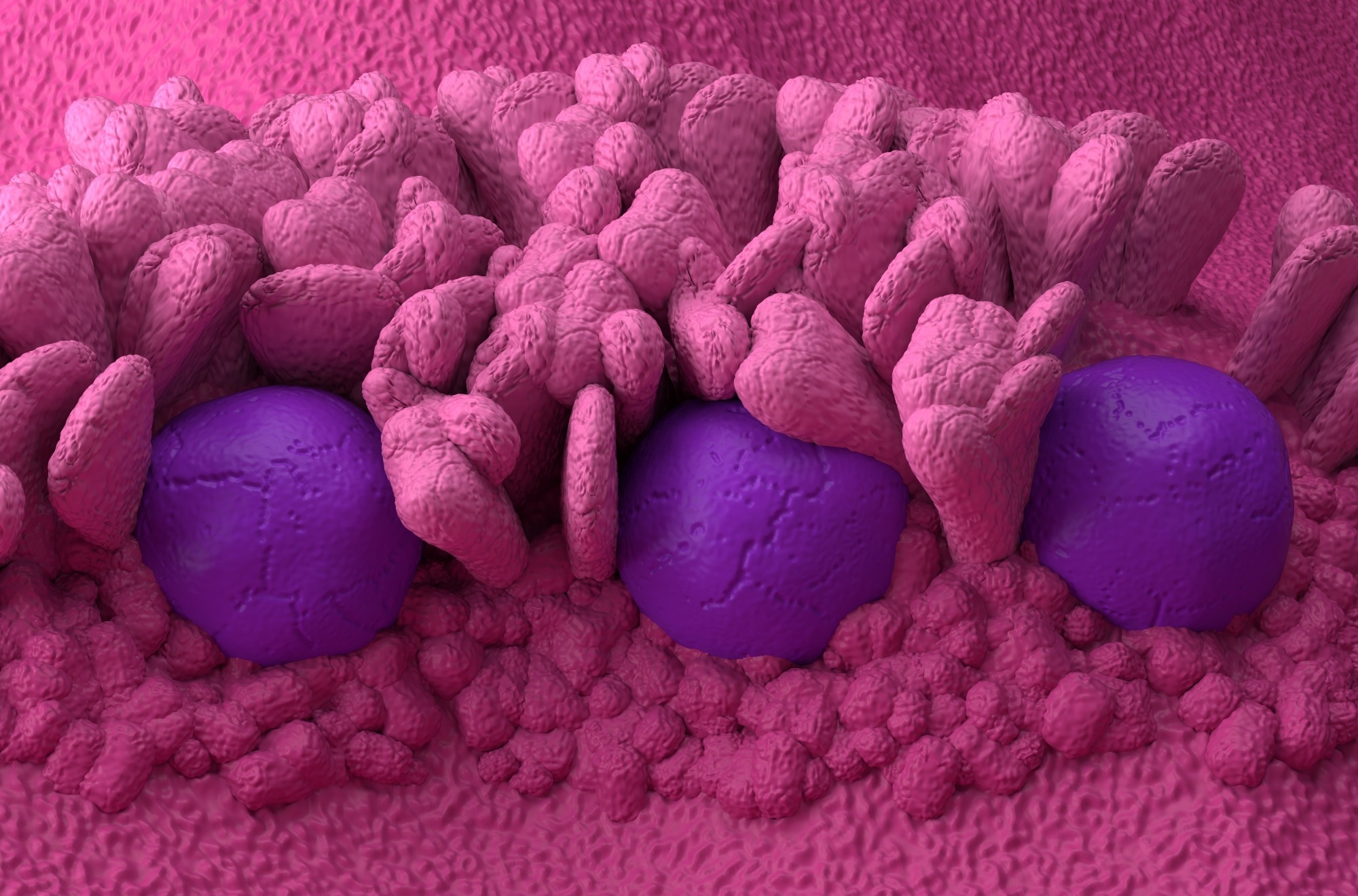
Study: Human gut M cells resemble dendritic cells and present gluten antigen. Image Credit: Nemes Laszlo / Shutterstock
In a recent study published in the journal Nature, researchers found that microfold (M) cells in the human gut resemble dendritic cells (DCs) and present antigens via the class II major histocompatibility complex (MHC-II). Notably, the study shows that MHC-II expression occurs constitutively and independently of interferon-gamma (IFNγ), distinguishing these cells from enterocytes, which require inflammatory cues for MHC-II induction and depend on IRF1 rather than the CIITA-dependent pathway used by M cells.
M cells are rare epithelial cells that reside in the follicle-associated epithelium of Peyer’s patches in the intestine and are involved in intestinal mucosal immunity. They transport luminal antigens to submucosal immune cells. Mouse M cells are derived from intestinal stem cells, require receptor activator of nuclear factor kappa-B ligand (RANKL), SRY-box transcription factor 8 (SOX8), Spi-B transcription factor (SPIB), and express glycoprotein 2 (GP2). However, human M cell differentiation is largely unknown.
Organoid Models Reveal Human M-Cell Development
In the present study, researchers developed an intestinal organoid model to study human M cells and establish their differentiation trajectory. The team optimized their previous culture protocol for human intestinal organoids by adding retinoic acid, RANKL, and tumor necrosis factor (TNF). This resulted in the appearance of GP2+ cells. SPIB reporter organoids were cultured in this medium, resulting in the efficient generation of SPIB-expressing cells.
Flow cytometry and immunofluorescence staining revealed SPIB expression in over 75% of cells, with around 3% co-expressing GP2. The co-expressing cells also expressed other M cell markers, such as C-C motif chemokine ligand 23 (CCL23) and SOX8. Organoid-derived cells were sorted by fluorescence-activated cell sorting (FACS) for single-cell ribonucleic acid sequencing (scRNA-seq) analysis.
A published scRNA-seq dataset was reanalyzed to identify primary M cell marker genes. This dataset was incorporated into other scRNA-seq resources covering all other intestinal cell types. The researchers determined a core set of primary M cell markers, including SPIB, GP2, SOX8, platelet-activating factor receptor (PTAFR), GABA receptor subunit pi (GABRP), and solute carrier family 2 member 6 (SLC2A6). These markers were highly expressed in organoid M cells.
Stages of Human M-Cell Differentiation
Over 90% of GP2+ organoid M cells expressed intercellular adhesion molecule 2 (ICAM2). However, ICAM2 was also expressed by half of the GP2- cells. Furthermore, SPIB+ M-lineage organoid cells could be stratified into ICAM2+ and ICAM2- subsets. Thus, M-lineage cells could be distinguished by three stages: SPIB+ICAM2-GP2- early M cells, SPIB+ICAM2+GP2- immature M cells, and SPIB+ICAM2+GP2+ mature M cells. These populations were sorted for transcriptomic profiling.
ICAM2+ cells were enriched in immature M cell markers, including CCL23, SOX8, and TNF-alpha-induced protein 2 (TNFAIP2). M cell maturation coincided with the appearance of RANKL-responsive genes. The team identified 1,639 differentially expressed genes (DEGs) during M cell differentiation. A gene ontology (GO) analysis, based on upregulated and downregulated DEGs in M cells, revealed that M cells and enterocytes were the most relevant cell types.
M cell organoids did not show markers for other intestinal cell types. Further, the team speculated that M cells and DCs might share a RANKL-induced transcriptional regulatory network, given that various RANKL-induced transcription factors of M cells are known from DC biology and that RANKL is essential for DC activation. The researchers focused on RUNX family transcription factor 2 (RUNX2), a RANKL-induced M cell transcription factor, which, like SPIB, is a master regulator of DCs.
RANKL, RUNX2 Axis Drives M-Cell Maturation
The addition of a RUNX2 inhibitor dose-dependently reduced the number of GP2+ M cells. Moreover, RUNX2 knockout resulted in a significant reduction of GP2+ organoid M cells. Further, the team explored the dataset for receptors expressed by M cells. M cells expressed the receptors of retinoic acid, RANKL, and TNF, consistent with their functional effects. FACS-based screening was subsequently performed to identify niche factors that promote M cell maturation.
Among 12 tested ligands, colony-stimulating factor 2 (CSF2) increased GP2+ organoid M cells by more than fourfold. Primary human M cells also expressed the CSF2 receptor, suggesting a potential in vivo function. Given the shared signaling regulators and transcription factors between DCs and M cells, the researchers explored additional DC genes in the scRNA-seq dataset. The team observed the induction of lymphoid DC marker genes during the maturation of M cells.
Further, scRNA-seq datasets of primary intestinal epithelial cells and several immune cell types were integrated. Unsupervised clustering analysis revealed a unique cluster of lymphoid DCs and M cells. Signature genes of this cluster included lymphoid DC markers that were expressed by both M cells and lymphoid DCs. A GO analysis based on upregulated DEGs in M cells revealed antigen-presenting cells (APCs) and activated DCs as the most closely related cell types.
M Cells Exhibit Dendritic-Like APC Features
Further, the morphology of FACS-sorted M cells was distinct from that of SPIB- cells in culture, with protrusions resembling those of DCs. Additionally, MHC-II gene expression increased during M cell maturation, as confirmed by flow cytometry, which showed MHC-II protein expression in both GP2+ and GP2- M cells. Of note, SPIB+ M-lineage cells expressed MHC-II proteins, while SPIB- cells did not.
Intestinal organoids cultured without M cell-inducing factors did not express MHC-II without IFNγ. However, organoid M cells exhibited spontaneous MHC-II expression in the absence of IFN-γ, reflecting a homeostatic antigen-presenting capacity not observed in enterocytes unless exposed to inflammatory cytokines, and with MIIC structures that are more developed and dendritic cell-like than those seen in IFNγ-stimulated enterocytes. Next, the team investigated the presence of the MHC-II compartment (MIIC), the hallmark of antigen presentation, using immunoelectron microscopy.
Structures representing early, multivesicular, intermediate, and multilaminar MIICs were observed in M cells, which resembled corresponding structures in DCs. Like DCs, M cells expressed components of the antigen processing and presentation machinery as well as various pattern recognition receptors. Importantly, M cells also expressed high levels of transglutaminase 2 (TGM2), enabling the deamidation of gliadin peptides into the disease-driving forms that bind HLA-DQ2.5.
Finally, a T cell-organoid co-culture assay focusing on T cell activation in celiac disease, an autoimmune disorder, confirmed that M cells process and present the gluten antigen. The study further demonstrated that TGM2 inhibition or TGM2 knockout reduced T cell activation, that M cells could activate naive CD4+ T cells under defined stimulatory conditions, and that they upregulated co-stimulatory molecules such as CD80 and CD86, reinforcing their classification as professional APCs.
Implications for Immunity and Celiac Disease
Taken together, human M cells share similarities with DCs and function as professional, non-hematopoietic APCs. Mouse M cells do not express MHC-II, and therefore, M cell-mediated antigen presentation may be unique to humans.
Given the low IFNγ levels and limited microbial exposure in the fetal and neonatal gut, M cells may function as early APCs in the intestinal epithelium through constitutive MHC-II expression.
M cells also process and present the gluten antigen, including its TGM2-dependent deamidated forms, suggesting a central role for these cells in celiac disease. However, the authors note that although the organoid findings are compelling, the full contribution of M cells to antigen presentation in vivo remains to be established within the complex lymphoid microenvironment of the intestine.
Journal reference:
- Wang, D., Lim, S., J., W., Okura, Y., Mizoroki, A., Spoelstra, W. K., Dayton, T., Van Son, G. J., Pronk, A., Smakman, N., C., G. B., Withoff, S., Jonkers, I. H., Van Zon, J. S., Tans, S. J., Peters, P. J., Van Es, J. H., & Clevers, H. (2025). Human gut M cells resemble dendritic cells and present gluten antigen. Nature, 1-10. DOI: 10.1038/s41586-025-09829-8, https://www.nature.com/articles/s41586-025-09829-8