The angiotensin-converting enzyme 2 (ACE2) enzyme attached to the membranes of cells is the entry point for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). They are abundantly found all over the body and most prominently in the lungs and nose. This coincides with initial symptoms exhibiting loss of smell and respiratory problems. Another early symptom of SARS-CoV-2 infection is loss of taste, although the mechanism of why this happens is unclear. New research led by Josephine M. Egan of the National Institute on Aging/Intramural Program found taste receptors have ACE2 and are also at risk for SARS-CoV-2 invasion.
Understanding the presence of viral infection in taste buds could help treat people with long COVID who could continue to experience loss of taste or gustatory changes months after recovering from infection.
The researchers write:
“By demonstrating the co-localization of SARS-CoV-2 virus, Type II taste cell marker, and the viral receptor ACE2, we show evidence for replication of this virus within taste buds that could account for acute taste changes during active COVID-19. This work also shows that the proliferation of the taste stem cells in recovering patients may take weeks to return to their pre-COVID-19 state, providing a hypothesis for more chronic disruption of taste sensation, reports of which are now appearing in the medical literature.”
The study “Human Taste Cells Express ACE2: a Portal for SARS-CoV-2 Infection” is available as a preprint on the bioRxiv* server, while the article undergoes peer review.
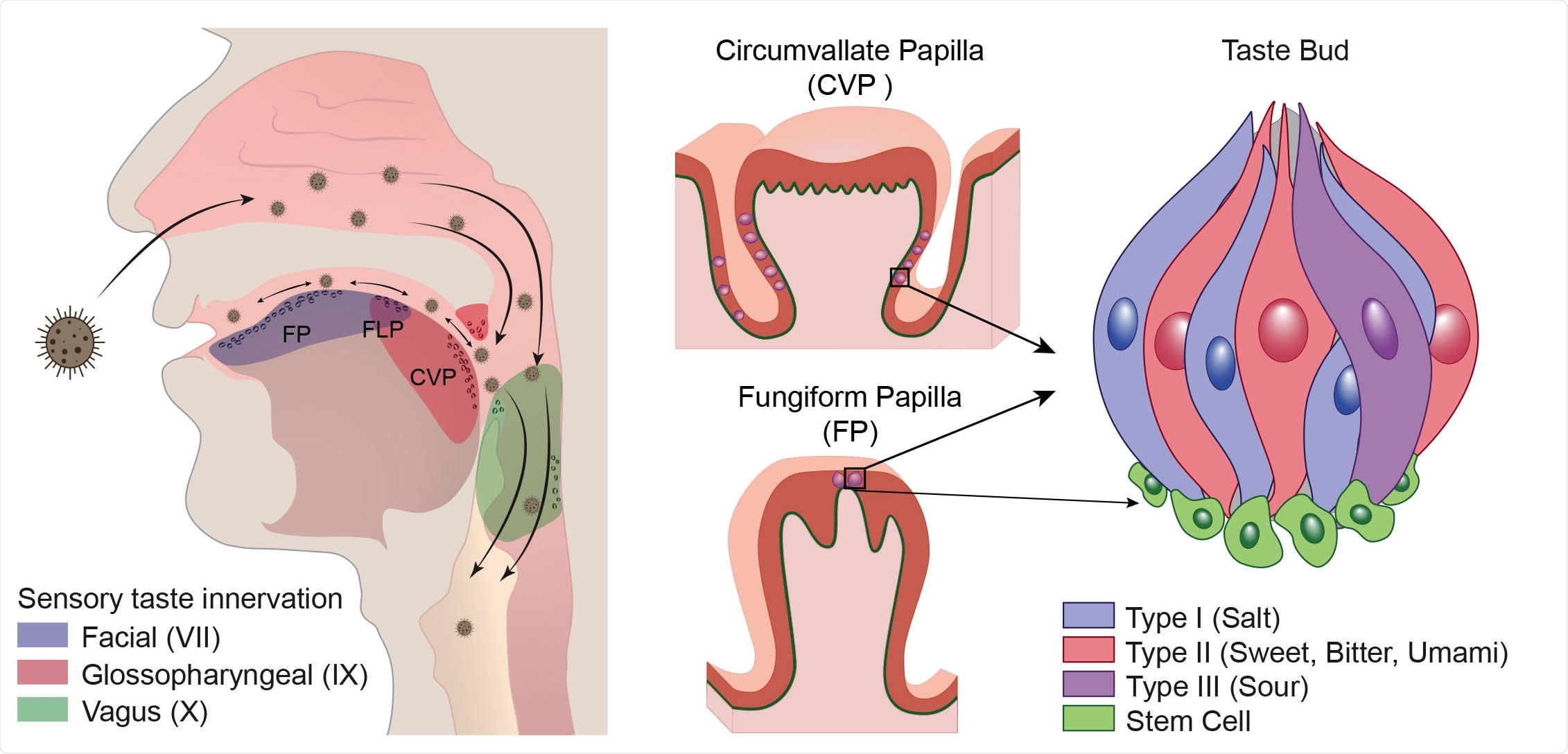
The receptor for SARS-CoV-2 angiotensin converting enzyme 2 (ACE2) is on Type II taste bud cells in taste papillae of the tongue. Panel A shows the distribution of taste buds and chemosensory cells in the oropharyngeal cavity and how inhaled virus may infect the tongue and oropharyngeal areas. Branches of three cranial nerves (CN VII, IX and X) are involved in relaying taste information to the central nervous system. Taste is first discriminated in taste receptor cells (TRCs) within taste buds located in circumvallate (CVP), foliate (FLP) and fungiform papillae (FP) in the tongue. Three defined TRCs relay five prototypic tastes. Stem cells immediately surrounding the taste bud receive signals from taste cells prompting differentiation into a replacement TRC. Circles on tongue, uvula, epiglottis and oropharyngeal areas represent taste buds and chemosensory cells.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
ACE2 present in Type II taste receptor cells
Researchers identified 5,000 to 10,000 taste buds, with almost half located at the base of the tongue called circumvallate papillae. In post-mortem tissue, they found ACE2 was coexpressed with phospholipase C β2 used in the signaling of type II taste receptor cells.
ACE2 was also discovered in taste receptor cells in the back of the tongue, a region known as fungiform pallipae, giving further evidence of a viral entry point for SARS-CoV-2.
“Replication of virus can likely then occur undisturbed and allow for transmission from the taste bud into circulation, and locally infect lingual and salivary gland epithelium, oral mucosa and larynx and even on into the lungs.”
Case studies of altered taste buds during COVID-19 infection
Researchers took samples of the fungiform pallipae — with one region containing taste buds — in a 45-year-old woman with controlled hypertension and who had presented with SARS-CoV-2. During her course of infection, she reported changes in her sense of taste, including not being able to taste the sweetness from chocolate and describing curry as ‘white.’
Her tongue was physically enlarged and redder around the fusiform pallipae than in a separate examination three months before.
The team confirmed the presence of SARS-CoV-2 RNA in the fusiform pallipae area, specifically in PLCB2 positive cells. The virus was also found in the lamina propria with disruptions in the stem cell layer. Six weeks after symptoms improved, which coincided with the patient’s recovery of sense of taste.
Another patient was a 63-year-old man with no preexisting conditions who had donated samples of his fusiform pallipae in 2019 before the pandemic. More samples were taken six weeks after he tested positive for COVID-19 infection. Though he experienced several long COVID symptoms, including mild loss of taste — coffee tasted like mud, and he could not taste chocolate. Samples of his fusiform pallipae 10 weeks after infection showed no presence of the virus. However, compared to his 2019 samples, he had altered changes to the stem cell layer of the tongue.
Based on the results, the researchers suggest impairments in stem cells may affect turnover and could contribute to the delayed recovery of sense of taste.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources