The high degree of variability observed in coronavirus disease 2019 (COVID-19) severity is characterized by extreme dysregulation in the host immune response, with disruptive immune activation seen at each stage of disease progression.
Autoantibodies (AABs) mistakenly target the hosts' own proteins. Recent reports have identified active AABs in those with severe COVID-19 that are clinically similar to those seen in classic autoimmune diseases, such as lupus and multiple sclerosis.
In a paper recently published on the preprint server medRxiv*, the association between COVID-19 and autoimmunity is investigated at all levels of disease severity. Herein, the researchers found that autoimmune responses are triggered following even mild and asymptomatic infection.
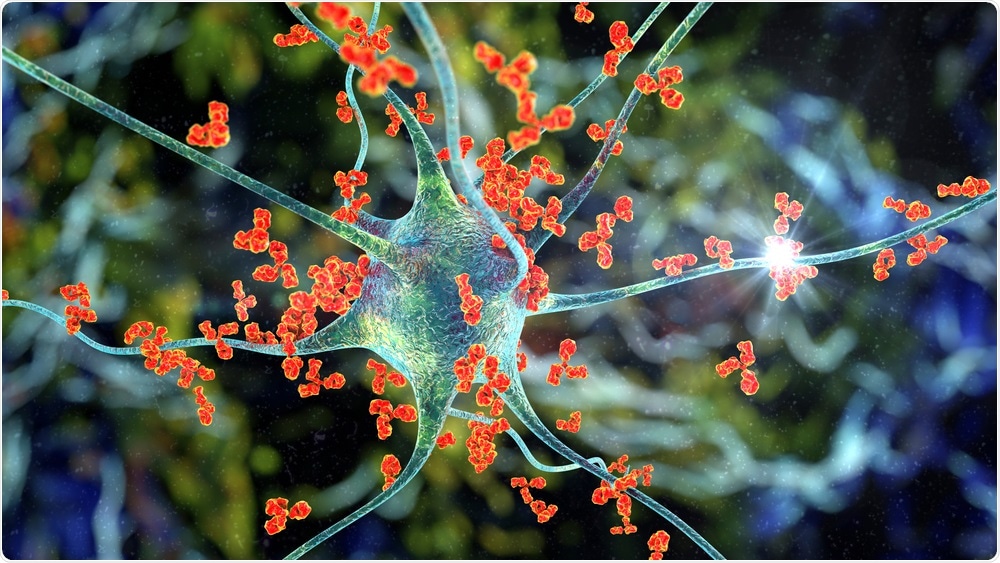 Study: Paradoxical Sex-Specific Patterns of Autoantibodies Response to SARS-CoV-2 Infection. Image Credit: Kateryna Kon / Shutterstock.com
Study: Paradoxical Sex-Specific Patterns of Autoantibodies Response to SARS-CoV-2 Infection. Image Credit: Kateryna Kon / Shutterstock.com

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Autoantibody expression induced by COVID-19
In total, 177 healthcare workers were enrolled in the study who had tested positive for SARS-CoV-2 immunoglobulin g (IgG) and had declared COVID-19 symptoms within the last six months. Each participant was categorized based on the time of sampling from the last reported symptoms and severity of symptoms. Additionally, 6 patients with lupus were also admitted to the study as a positive control for AABs.
An AAB array bearing 91 protein antigens was developed, allowing the group to quantify a variety of cytokines, lung-specific proteins, and other proteins known to interact with SARS-CoV-2. These antigens were in addition to a selection of AAB-antigens observed in systemic sclerosis and other similar inflammatory conditions.
Of the 177 healthcare workers enrolled in the study, the presence of at least one AAB was detected in 160. On average, each had 5.2 reactive AABs in their sera, where 9% had none, 36% had 1-2, 29% had 3-6, and 25% had more than 6.
As compared to healthy controls, however, this difference did not meet the threshold of statistical significance (5.2 AABs per person compared to 2.3). As expected, the participants with lupus exhibited much greater odds of bearing significantly more AABs with an average of 17.3 AABs.
Age, sex, and timing of reported symptoms were not found to correlate with IgG levels in the participants. However, the reactivity of IgG towards 12 of the 91 antigens included in the panel differed significantly from healthy controls. The identified antigens have previously been implicated in a number of immune-mediated inflammatory diseases, and also included organ-specific autoantibody targets in the thyroid and islet cells.
Autoantibody symptom correlation
The prevalence of certain antibodies correlated with symptoms, finding that the presence of AABs against CHD3 was associated with skin changes. Moreover, AABs against CHD3 were reported in 19% of those positive for these AABs, as compared to 5% without.
Other correlations included shortness of breath, where 56% of those with anti-SRP19 AABs reported the symptom as compared to 28% of those without. Additionally, diarrhea was present in 52% of those with anti-IFNA4 AABs and only 27% of those without. Interestingly, positivity for anti-INS AABs correlated with the early reporting of symptoms, but negatively with the development of fever.
Increased reactivity to interferon and S100A8/S100A9 was also found amongst those with prior SARS-CoV-2 infection at a greater incidence than naïve individuals. Notably, S100A8/S100A9 is expressed by immune cells in response to environmental triggers and cellular damage.
The presence of these cytokines is strongly associated with poor clinical outcomes in patients with severe pulmonary disease. Several other indicators of inflammation were also upregulated in those with prior COVID-19.
Study takeaways
Previous reports have demonstrated that the immune response is disrupted and modulated by COVID-19, and that the generation of AABs occurs and may contribute significantly to severe disease states.
This study has further demonstrated that AABs associated with other autoimmune diseases may also be detected in those with a prior mild infection, which could be a precursor to underlying autoimmune disease as a direct result of COVID-19. The presence of AABs may have no clinical significance for positive individuals; however, the researchers of the current study highlight the need for ongoing surveillance of AABs induced by COVID-19 in long-term studies.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Liu, Y., Ebinger, J. E., Mostafa, R., et al. (2021). Paradoxical Sex-Specific Patterns of Autoantibodies Response to SARS-CoV-2 Infection. medRxiv. doi:10.1101/2021.07.15.21260603. https://www.medrxiv.org/content/10.1101/2021.07.15.21260603v1
- Peer reviewed and published scientific report.
Liu, Yunxian, Joseph E. Ebinger, Rowann Mostafa, Petra Budde, Jana Gajewski, Brian Walker, Sandy Joung, et al. 2021. “Paradoxical Sex-Specific Patterns of Autoantibody Response to SARS-CoV-2 Infection.” Journal of Translational Medicine 19 (1). https://doi.org/10.1186/s12967-021-03184-8. https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-021-03184-8.