Researchers in the United States and China have developed plasmid DNA immunogens that induce effective antibody responses in mice against the spike protein of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) – the agent that causes coronavirus disease 2019 (COVID-19).
Although the spike protein is highly immunogenic, the majority of antibodies do not target amino acids in the main functional motif of the RBD (RBM) that interacts with ACE2.
Now, a team – from the University of California San Diego, La Jolla Institute for Immunology in California, Capital Medical University in Beijing, and the Chinese Academy of Sciences in Beijing – have generated plasmid DNA (pDNA) immunogens comprising contact residues in the RBM ridgeline that play a key role at the RBM: ACE2 interface.
Maurizio Zanetti and colleagues report that priming mice with these immunogens induced a primary and memory antibody response against the RBD.
Antibodies expanded by a booster immunization with a recombinant spike protein were highly effective at neutralizing the ancestral (WA1/2020) strain of SARS-CoV-2, as well as the B.1.351 (beta) and B.1.617.2 (delta) variants of concern.
The team says the findings demonstrate that immunogens based on structure selection can focus the response to conserved sites of vulnerability shared between different viral strains and induce neutralizing antibodies across variants of concern.
A pre-print version of the research paper is available on the bioRxiv* server, while the article undergoes peer review.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Systematic vaccine deployment the most promising approach to controlling the COVID-19 pandemic
While non-pharmaceutical interventions (NPIs) such as social distancing, travel restrictions and lockdowns have reduced the transmission of SARS-CoV-2, they are difficult to sustain due to the negative social and economic impacts.
Furthermore, NPIs alone have not been sufficient to control the global pandemic, which has infected more than 234 million people and caused 4.79 million deaths since it began in late December 2019.
The systematic deployment of vaccines to generate a protective population or “herd” immunity represents the most promising approach to containing viral transmission and combatting the pandemic.
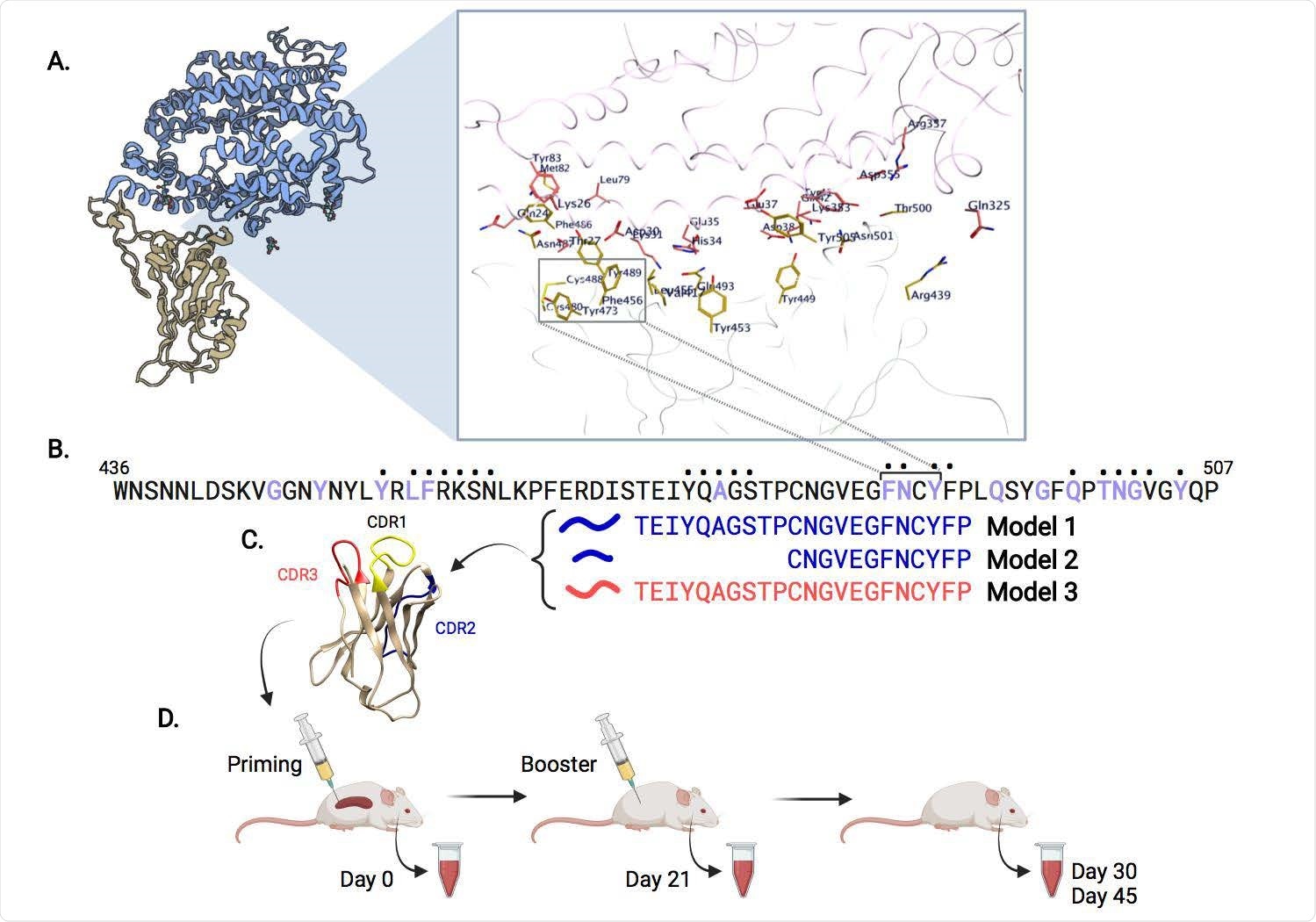
Overview of SARS-CoV-2 epitope selection, protein engineering, and immunization. (A) SARS-CoV-2 Spike protein (yellow) interacting with ACE2 (blue), PDB ID: 6M0J. A zoomed view shows SARS-CoV-2:ACE2 interacting residues. (B) Spike protein RBM (436-507) sequence. Purple residues indicate ACE2 binding, dots above residues indicate B38 or CC12.1 antibody binding. Immunogens models 1-3 span the putative B cell epitope FNCY (486-489). (C) VH62 model with CDR1 (yellow), CDR2 (blue), CDR3 (red). (D) Timeline of priming (day 0), and booster shot (day 21), with blood draws (days 0, 21, 30, 45).
More about the spike RBD and RBM
The receptor-binding motif (RBM) ridgeline of the SARS-CoV-2 spike RBD contributes key amino acid residues involved in the interaction with the human ACE2 receptor.
While the RBM is a target of potent neutralizing antibodies isolated from individuals who have recovered from SARS-CoV-2 infection, more than 80% of the whole antibody response in convalescents is predominantly directed to sites that lie outside of the RBD.
Zanetti and colleagues say this is consistent with the observation that B and T cell responses targeting the RBD, and in particular the RBM, are markedly less frequent than the total response to spike.
All but one of the 20 most potent neutralizing antibodies characterized to date binds to the RBM and blocks attachment to ACE2.
What did the current study involve?
In an effort to concentrate the antibody response to the RBM, the researchers used protein engineering to generate three pDNA immunogens expressing a B cell epitope that spans 22 amino acids of the RBM ridgeline and encompasses the 486Phe-Asn-Cys-Tyr489 patch.
This patch contributes key contact residues to ACE2 binding and is targeted by some of the most potent human class 1 neutralizing antibodies.
Priming of C57BL/6 mice with these pDNAs induced primary and memory antibody responses against the spike RBD.
Booster immunization with a recombinant spike protein yielded a rapid memory response, with immune sera antibodies binding strongly to the purified RBD and the spike protein.
The pDNAs were primed for consistent response across different viral strains. Antibodies expanded by the booster immunization were highly effective at neutralizing the ancestral WA1/2020 virus, as well as the beta and delta variants of concern.
Conformational analysis of SARS2-CoV-2 RBM structure and predicted conformation of VH Model 2. In the Spike S1 protein (A) the tip of the RBM ridgeline is shown in dark green and the FNCY patch in dark blue. In Model 2 (ribbon B) and (space-filling C) the modeled CDR2 loop is shown in dark green, while the grafted RBM epitope is in dark blue. Panels on the right show the interface between ACE2 and SARS-CoV-2 RBM (D), and ACE2 and the CDR2 loop of Model 2 (E). Color scheme: A: gray - RBD; green - RBM; blue – ACE2 contact residues; B and C: yellow -CDR1; green - CDR2; orange - CDR3; blue - SARS-Cov-2 RBM residues grafted in CDR2; gray - tetanus toxoid epitope; D: pink - ACE2; green - SARS-Cov-2 RBM residues; E: pink - ACE2; blue - SARS-Cov-2 RBM residues grafted in CDR2.
What are the implications of the study?
Zanetti and colleagues say the results suggest that this pDNA-protein (prime-boost) approach can focus anti-SARS-CoV-2 responses to a narrow region of the RBM and induce neutralizing antibodies across variants.
The researchers also warn that achieving global control of the COVID-19 pandemic will require the development of vaccines that overcome obstacles such as antigen stability, vaccine thermostability, and the logistics of cold chain requirements.
“pDNA vaccines of the type presented here offer such a possibility,” says the team. “For instance, they can be incorporated in thermostable needle-free delivery vehicles for global and equitable vaccination.”

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Zanetti M, et al. Structure selected RBM immunogens prime polyclonal memory responses that neutralize SARS-CoV-2 variants of concern. bioRxiv, 2021. doi: https://doi.org/10.1101/2021.10.01.462840, https://www.biorxiv.org/content/10.1101/2021.10.01.462840v1
- Peer reviewed and published scientific report.
Almanza, Gonzalo, Alex E. Clark, Valentina Kouznetsova, Eduardo Olmedillas, Andrea Castro, Igor F. Tsigelny, Yan Wu, et al. 2022. “Structure-Selected RBM Immunogens Prime Polyclonal Memory Responses That Neutralize SARS-CoV-2 Variants of Concern.” Edited by Charles R. M. Bangham. PLOS Pathogens 18 (7): e1010686. https://doi.org/10.1371/journal.ppat.1010686. https://journals.plos.org/plospathogens/article?id=10.1371/journal.ppat.1010686.