Since the beginning of the pandemic, governments and healthcare experts have been warning that 'at-risk' individuals stand to suffer far more from coronavirus disease 2019 (COVID-19) than generally healthy individuals, and they show a far higher chance of progressing to severe disease, hospitalization and death.
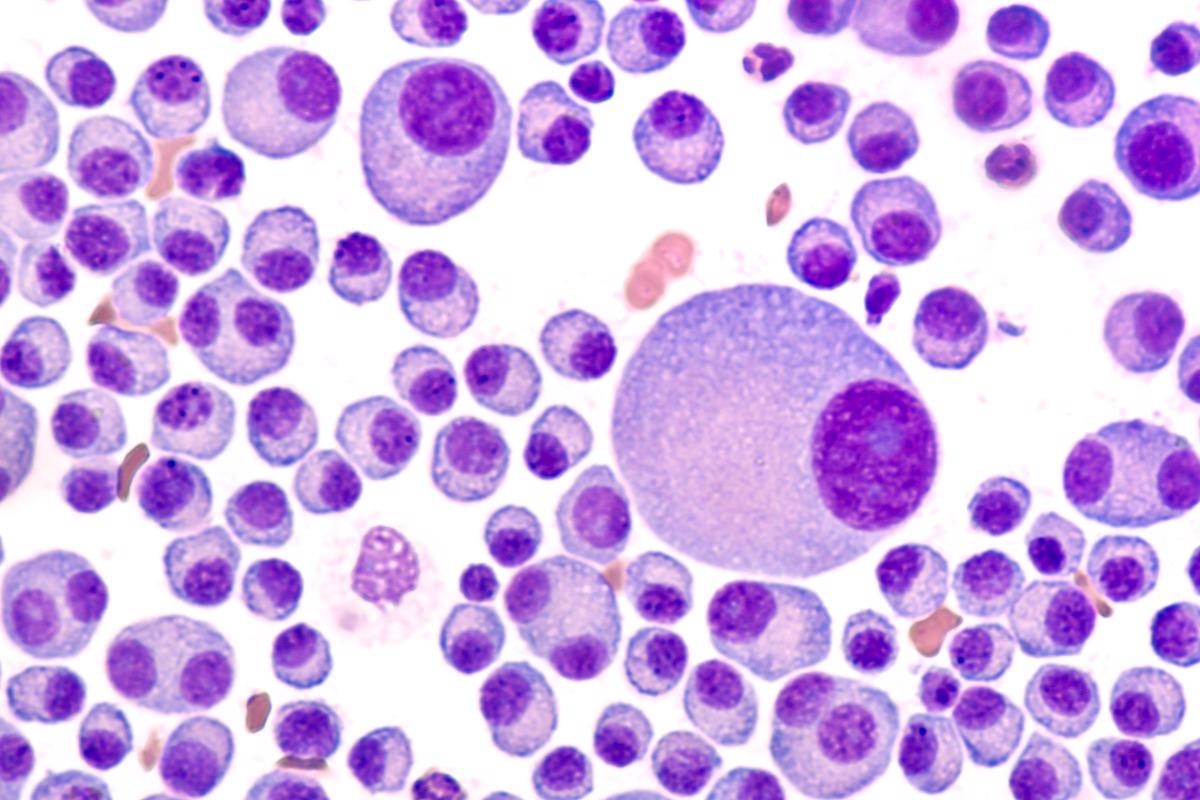 Study: Impact of Omicron variant on the response to SARS-CoV-2 mRNA Vaccination in multiple myeloma. Image Credit: David A Litman/Shutterstock
Study: Impact of Omicron variant on the response to SARS-CoV-2 mRNA Vaccination in multiple myeloma. Image Credit: David A Litman/Shutterstock

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
While vaccination has significantly reduced these risks for healthy individuals as well as many 'at-risk' groups, many are still unsure of the level of protection that the vaccine offers the immunocompromised.
Researchers from the University of Parma have been investigating the protection offered by the vaccine in patients suffering from multiple myeloma, and have posted their results to the medRxiv* preprint server.
Background
Only patients from the Hematology Unit of Parma Hospital were eligible for inclusion within the study. A total of 40 patients suffering from multiple myeloma (MM) consented to be part of the study - six of these suffered from monoclonal gammopathies of undetermined significance (MGUS),10 were smoldering myeloma (SM) patients, and the remaining 24 were either newly diagnosed MM (MMD) or relapsed-refractory MM (MMR). The researchers gathered peripheral blood (PB) samples before the first dose of the vaccine, and then two weeks after the second dose. Individuals were vaccinated with the Pfizer-BioNTech BNT162b2 mRNA vaccine. Sixteen patients with MM were also given a heterologous booster dose using the Moderna mRNA-1273 vaccine, and blood samples were taken again 14 days after this.
Two patients had to be excluded from the final analysis, one who showed pre-existing antibodies, and one who caught COVID-19 during the study. The patients showed an overall seropositivity rate of 86.8% for anti-spike IgG antibodies. Five patients showed no detectable antibodies. All five of these had immunoparesis in 2/3 Ig classes, which was associated with lower spike-IgG-Abs. Generally, the researchers found that MMR patients tended to show much lower antibody titers compared to the other disease variants.
Pseudovirus neutralization assays examining the response to the vaccine homologous spike protein showed that MMR patients also had significantly lower neutralizing antibody titers compared to patients suffering MGUS, SMM and MMD. Out of a total of six patients that showed no detectable neutralization titer, five were MMR patients. These pseudovirus neutralization assays were then expanded to test the patients’ sera ability to neutralize different variants spike proteins, including Alpha, Beta, Gamma, Delta and Omicron. Significant correlations between the levels of antibody initially detected in the sera and the neutralization titers indicate that the vaccines retain at least a certain amount of efficacy against the variants in these patients. MGUS patients appeared to show the most significant reductions in neutralizing antibody titers for the Beta and Omicron variants, while SMM and MMD patients showed generally decreased Nab titers to all variants. MMR patients showed even lower responses to Beta, Delta and Omicron variants than they did to the initial Wuhan-Hu-1 spike protein.
When examining the responses to the booster vaccine in the 16 MM patients, it became clear that MMR patients still show significantly lower responses than MMD patients. However, the booster does still appear to have a beneficial effect, with six out of seven MMD patients showing improved spike-IgG-Abs levels, and three out of five seropositive MMR patients showing improvement. Even more telling, half of the MMR patients who registered as seronegative following the second vaccine dose underwent seroconversion. While MMR patients showed no significant improvement in neutralizing antibody titer following the booster, MMD patients did. This was seen against all spike proteins, including Omicron, for MMD patients, while MMR patients showed improved titers against the Alpha, Gamma and Delta variants, but not the Beta or Omicron variants. However, four MMR patients who previously showed no detectable titers against the Omicron variants reached detectable levels following the booster.
Conclusion
The authors highlight that they have successfully shown that MM patients with (MMR) have reduced spike-specific antibody levels as well as neutralizing titers following full mRNA vaccination, and that this was seen for all variants analyzed.
They also showed that booster immunization can help to alleviate the reduced response to vaccines in newly diagnosed MM patients and in some MMR patients. Omicron in particular shows a significant threat to MMR patients. This information could be critical for healthcare workers, multiple myeloma patients, and specialists and could help inform these individuals of the specifics of the risk they face.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources