The coronavirus disease 2019 (COVID-19) pandemic was caused by the emergence of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
SARS-CoV-2 causes mild to severe infection, with severely infected patients, often admitted to intensive care units (ICUs). Patients experiencing severe COVID-19 are at an increased risk of secondary fungal and bacterial infections.
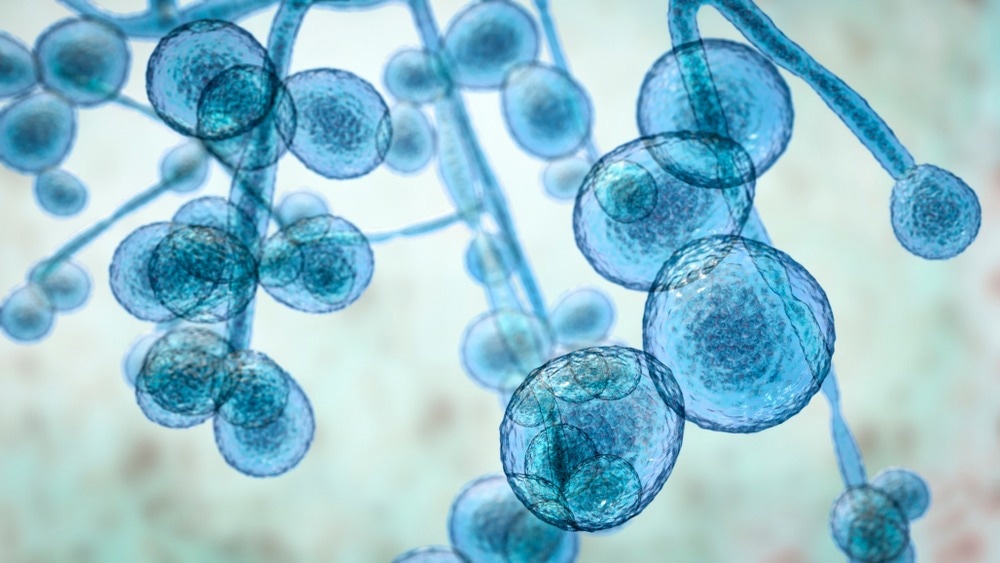
Study: Antifungal therapy in the management of fungal secondary infections in COVID-19 patients: A systematic review and meta-analysis. Image Credit: Kateryna Kon / Shutterstock.com
Background
Some commonly reported secondary fungal infections that are associated with an increased rate of mortality and morbidity include COVID-19-associated pulmonary aspergillosis (CAPA), mucormycosis (CAM), and invasive candidiasis. These infections are caused by pathogens belonging to Rhizopus, Aspergillus, and Candida species, respectively.
Prior research has shown that secondary fungal infections in COVID-19 patients are high. Moreover, 14.8% and 33% of mild and severe COVID-19 patients, respectively, develop fungal secondary infections.
Notably, COVID-19 patients who are also receiving treatments for cancers, diabetes mellitus, or immunosuppressive agents are at a higher risk of fungal co-infections when hospitalized.
The time interval between COVID-19 diagnosis and the development of secondary fungal infections varies significantly among patients. As fungal co-infections increase the risk of mortality in COVID-19 patients, early detection and treatment are important to reduce adverse clinical outcomes.
Although there are no definitive guidelines available to manage secondary fungal infections in patients infected with SARS-CoV-2, an abundance of evidence based on case series and cohort studies is available and can help manage this condition. The most common antifungal therapies (AFTs) used to treat these infections include echinocandins, liposomal amphotericin B, and azole.
About the study
In a recent PLoS One journal study, researchers systematically analyzed published literature to explore the frequency of secondary fungal infections among COVID-19 patients. Herein, they describe secondary fungal infections as those caused by fungal species at the time of hospital admission or during the period of hospital stay. The authors further studied the effectiveness of AFTs in treating COVID-19 patients with fungal co-infection.
In the current study, the researchers performed a comprehensive literature search using several search engines, including Scopus, PubMed, Cochrane Library, Web of Sciences, ClinicalTrial.gov, medRxiv.org, Google scholar, and bioRxiv.org to obtain relevant studies related to AFTs for secondary fungal infection management in COVID-19 patients.
The researchers followed the PRISMA 2009 statement for reporting systematic reviews and meta-analysis data. Furthermore, they obtained relevant prospective and retrospective studies, case series, clinical trials, and clinical reports associated with fungal coinfection in COVID-19 patients. The Mantel Haenszel random-effect model was used to predict the pooled risk ratio for the required outcome.
Study findings
One study reported that 28.2% of COVID-19 patients were diagnosed with secondary fungal infections during their hospital stay. This study estimated an overall mortality rate of 45.7% in the study cohort.
The mortality rate associated with CAPA and CAM was 75.2% and 13%, respectively. Comparatively, another study reported that the mortality rate associated with CAPA is lower than CAM.
Limited studies were available regarding the mortality rate of COVID-19-associated candidemia (CAC).
An Atlanta-based study reported 30.9% mortality in COVID-19 patients with secondary fungal infections. Several other studies have similarly indicated that as compared to those infected with SARS-CoV-2 alone, COVID-19 patients co-infected with fungal infections have a higher mortality rate.
Many European, Chinese, and Australian studies have reported that the most commonly diagnosed fungal infection in COVID-19 patients is CAPA, followed by CAC and CAM. Aspergillus fumigatus was identified as the most commonly occurring causal organism.
CAPA patients receive voriconazole as the first line of AFT and amphotericin B as the second line of treatment. The total duration of AFTs was between two and 90 days.
CAC mostly prevailed among the Chinese population, with these patients predominantly treated with echinocandins, azoles, and amphotericin B. Candida albicans was found to be the causal organism of CAC, with the duration of antifungal treatment ranging from four to 21 days.
CAM was the most prevalent agent responsible for secondary fungal infections in India. These infections were primarily managed with amphotericin B, either as a single drug or in combination with other antifungal drugs.
The total duration of AFTs for CAM was between 11 and 150 days. A higher survival frequency was observed among COVID-19 patients with secondary fungal infection subjected to AFTs as compared to those who were not receiving treatment.
Conclusions
One of the limitations of the current study is that it failed to highlight the most effective individual AFT or class of antifungal agents to treat COVID-19 patients with fungal co-infection. Furthermore, some of the reports included in this study failed to mention the exact antifungal drugs, dosage, duration of treatment, and other relevant information.
Nevertheless, the current study strongly indicated that CAC, CAPA, and CAM are the most common fungal secondary infections among COVID-19 patients. These patients are treated with fluconazole (CAC), voriconazole (CAPA), and liposomal amphotericin B (CAM).
Overall, the survival rate of treated patients was much higher compared to untreated patients.
Journal reference:
- Sah, S. K., Shariff, A., Pathakamuri, N., et al. (2022) Antifungal therapy in the management of fungal secondary infections in COVID-19 patients: A systematic review and meta-analysis. PLoS ONE 17(7). doi:10.1371/journal.pone.0271795.