PCC, often referred to as 'long COVID,' is a critical COVID-19 complication that has significantly impacted human lives globally. Further investigation on PCC risks post-COVID-19 vaccination and SARS-CoV-2 infections with novel VOCs is needed to guide policy-making, vaccination regimens, and other public health measures.
Study: Post COVID-19 condition after Wildtype, Delta, and Omicron variant SARS-CoV-2 infection and vaccination: pooled analysis of two population-based cohorts. Image Credit: Red-Diamond / Shutterstock.com

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
About the study
The current study analyzes PCC severity and prevalence among vaccinated and unvaccinated individuals infected with SARS-CoV-2 WT, Delta, or Omicron strains.
Data were obtained prospectively through online questionnaires from two cohorts diagnosed with COVID-19 between August 5, 2020, and February 25, 2022. In addition, the Zurich SARS-CoV-2 and Corona Immunitas seroprevalence study (fifth phase) cohorts were included.
The Zurich SARS-CoV-2 cohort included individuals who completed follow-up assessments six months post-SARS-CoV-2 infection. Conversely, from the Corona Immunitas study cohort, those who reported SARS-CoV-2 exposure during the Delta and Omicron waves and those who completed follow-up assessments six months post-most recent COVID-19 diagnosis, were included.
Sociodemographic characteristics, comorbidities, vaccination status, prior COVID-19 history, current symptoms, current health status, and the presence of PCC symptoms using a 23-item list of commonly reported symptoms were also provided.
The primary study outcome was self-reported COVID-19-related symptoms six months following the most recently diagnosed SARS-CoV-2 infection. Secondary outcomes comprised self-reported COVID-19-related symptoms and PCC severity based on the number of symptoms during follow-up assessments.
In the sensitivity analyses, patients were categorized with mild, moderate, or severe COVID-19 based on the EuroQoL visual analog scale (EQ-VAS). All Zurich SARS-CoV-2 cohort participants were categorized as WT-infected.
Infections between July 7, 2021, and December 31, 2021, were categorized as Delta VOC infections, whereas those from January 1, 2022, onward were classified as Omicron infections.
The medRxiv, EMBASE, and MEDLINE databases were searched without language restrictions between January 1, 2020, and August 29, 2022, for studies and systematic reviews that assessed PCC symptoms and prevalence after SARS-CoV-2 VOC infections among vaccinated and unvaccinated individuals.
All identified studies described PCC as symptoms experienced four weeks or less and over 12 weeks after COVID-19 diagnosis. These studies included hospitalized COVID-19 patients, healthcare workers (HCWs), and the United Kingdom ZOE symptom app users.
Multivariable and multinomial logistic regression models were used for estimating PCC risk reductions and severity, respectively, and the odds ratios (ORs) were calculated. In addition, exploratory hierarchical cluster analyses were performed to identify clusters of individuals with similar symptoms and evaluating differences in PCC presentation across VOCs.
Study findings
Data from 1,045 and 305 participants from the Zurich SARS-CoV-2 and Corona Immunitas cohorts, respectively, were analyzed. All individuals were followed up for a median of 183 days. The median ages of the corresponding cohort individuals were 51 years and 43 years, respectively, with 51% and 59% of the corresponding cohorts female.
About 25%, 17%, and 13% of WT-, Delta-, and Omicron-infected individuals, respectively, were affected by PCC six months after their most recent SARS-CoV-2 infection.
Among individuals vaccinated before infection, 15% and 11% experienced PCC after Delta and Omicron infections, respectively. No distinct patterns in PCC symptoms were observed across participants.
Omicron-infected and vaccinated individuals had lower PCC risks than WT-infected and unvaccinated individuals, with an OR 0.4, irrespective of COVID-19 severity. No significant differences were observed in the prevalence of PCC concerning vaccination doses received or the timing of the most recent vaccination, with sensitivity analyses showing similar results.
Strong evidence was obtained for a risk reduction in those documenting one or two PCC symptoms among those vaccinated against COVID-19 and infected with Omicron compared to unvaccinated WT-infected individuals (OR 0.4). Four PCC symptom clusters comprising neurocognitive, systemic, musculoskeletal, and cardiorespiratory symptoms were identified with identical patterns across VOCs, with malaise, headache, fatigue, and smell or taste disturbances prevalent across all clusters.
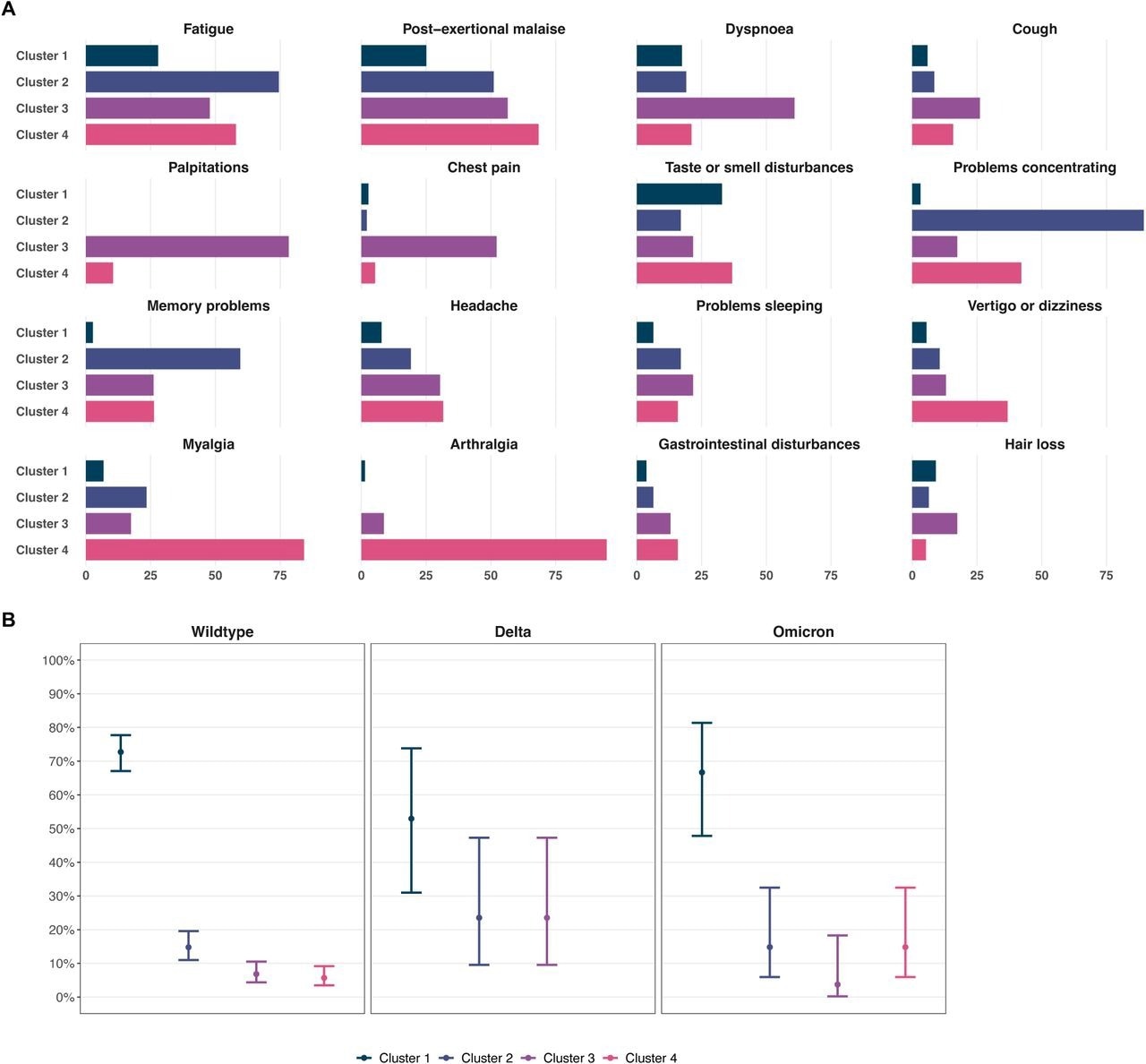 Prevalence of specific post-COVID-19 condition-related symptoms six months after SARS-CoV-2 infection across symptom clusters. Four clusters of individuals with post-COVID-19 condition six months after infection were identified based on multiple correspondences and hierarchical cluster analyses, consisting of individuals with (1) diverse systemic symptoms and lower symptom count and with (2) predominantly neurocognitive, (3) cardiorespiratory, or (4) musculoskeletal symptoms. Panel A depicts distributions of specific post-COVID-19 condition-related symptoms across clusters. Panel B shows the proportion of individuals belonging to each cluster across infections with Wildtype, Delta, and Omicron SARS-CoV-2. Points represent point estimates, and error bars represent 95% Wilson confidence intervals for estimated proportions.
Prevalence of specific post-COVID-19 condition-related symptoms six months after SARS-CoV-2 infection across symptom clusters. Four clusters of individuals with post-COVID-19 condition six months after infection were identified based on multiple correspondences and hierarchical cluster analyses, consisting of individuals with (1) diverse systemic symptoms and lower symptom count and with (2) predominantly neurocognitive, (3) cardiorespiratory, or (4) musculoskeletal symptoms. Panel A depicts distributions of specific post-COVID-19 condition-related symptoms across clusters. Panel B shows the proportion of individuals belonging to each cluster across infections with Wildtype, Delta, and Omicron SARS-CoV-2. Points represent point estimates, and error bars represent 95% Wilson confidence intervals for estimated proportions.
Of the 221 screened studies, four investigating the association of Delta or Omicron infections and 11 investigating the association of prior vaccination with PCC were included for the final analysis. Two studies reported lower PCC risk with Omicron infections than other VOC infections.
One study found a lower PCC risk with Alpha VOC infection than with WT infection. In contrast, eight studies reported a significantly lower PCC incidence among messenger ribonucleic acid (mRNA) and adenovirus vector vaccine recipients. Nevertheless, three studies found no differences between vaccinated and unvaccinated SARS-CoV-2-infected individuals.
Conclusions
Overall, the study findings showed that Omicron infection and receipt of COVID-19 vaccines reduced the risk of PCC symptoms six months following infection compared to WT infection without prior vaccination.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Ballouz, T., Menges, D., Kaufmann, M., et al. (2022). Post COVID-19 condition after Wildtype, Delta, and Omicron variant SARS-CoV-2 infection and vaccination: pooled analysis of two population-based cohorts. medRxiv. doi:10.1101/2022.09.25.22280333. https://www.medrxiv.org/content/10.1101/2022.09.25.22280333v1.
- Peer reviewed and published scientific report.
Ballouz, Tala, Dominik Menges, Marco Kaufmann, Rebecca Amati, Anja Frei, Viktor von Wyl, Jan S. Fehr, Emiliano Albanese, and Milo A. Puhan. 2023. “Post COVID-19 Condition after Wildtype, Delta, and Omicron SARS-CoV-2 Infection and Prior Vaccination: Pooled Analysis of Two Population-Based Cohorts.” Edited by Dong Keon Yon. PLOS ONE 18 (2): e0281429. https://doi.org/10.1371/journal.pone.0281429. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0281429.