How powerful is your plate? A Swedish study using advanced heart imaging reveals that diets low in fiber and high in red meat increase the risk of dangerous coronary artery plaques.
 Study: Low-fibre diet is associated with high-risk coronary plaque features. Image credit: ridersuperone/Shutterstock.com
Study: Low-fibre diet is associated with high-risk coronary plaque features. Image credit: ridersuperone/Shutterstock.com
A recent Swedish study analyzed the association between a low-fiber diet and coronary atherosclerotic plaque, a leading cause of early death. The paper was published in Cardiovascular Research.
Introduction
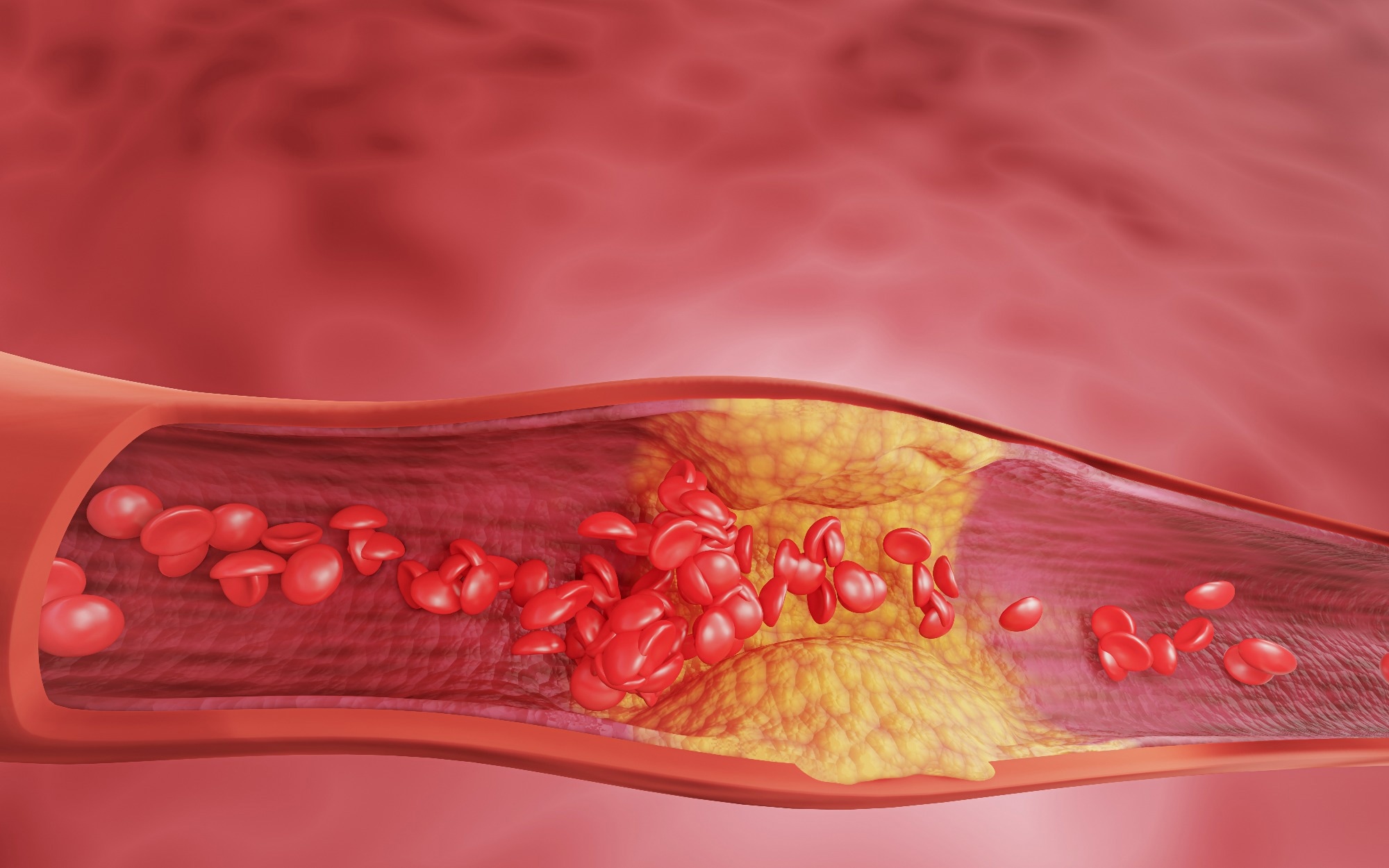
Globally, cardiovascular disease (CVD) is a major cause of death and disability. Coronary heart disease is responsible for most premature deaths due to CVD, mainly by the build-up of atherosclerotic fatty plaques over decades. These may rupture, blocking one or more arteries in the heart and causing a heart attack or sudden coronary death.
New methods are being investigated to identify plaques at risk of rupture. Coronary computed tomography angiography (CCTA) is an emerging technology that promises to be an accurate and non-invasive method of diagnosis. It is currently used internationally to assess the degree of risk the plaque poses.
The Mediterranean diet and other similar diets predict lower CVD risk. Much of this effect is due to their high fiber content. Dietary indices use multiple food items to compare diets for their health-related characteristics.
Kaluza et al. built an anti-inflammatory diet index (DI) using foods correlated to inflammatory markers like the high-sensitive C-reactive protein (hsCRP). This has been validated in Swedish prospective studies over 16 years of follow-up, where outcomes like death, abdominal aortic aneurysm, and heart failure were lower among people with a higher DI who consumed little pro-inflammatory foods.
Fruits, vegetables, nuts, whole-grain bread, breakfast cereals or oatmeal, canola and olive oil, coffee, tea, chocolate, red wine, and beer are among foods with anti-inflammatory characteristics. Conversely, potato chips, red meat, and sugary drinks are associated with systemic inflammation.
The current study employed a similar DI to explore the link with coronary atherosclerosis, coronary plaque risk by CCTA, and cardiovascular risk factors.
About the study
The current study used data from the Swedish CArdioPulmonary BioImage Study (SCAPIS), including 24,079 adults between 50 and 64 years. All were free of clinical cardiovascular disease at baseline. They responded to an invitation to participate in the study sent to a randomly selected population sample.
Their diet was analyzed using the dietary index (DI), which is primarily based on the content of plant-based foods and low in inflammatory foods like processed or red meat and sugary drinks. The healthiest group was in the highest tertile of the dietary index, reflecting more plant-based and anti-inflammatory foods, while the lowest tertile reflected diets high in inflammatory foods.
CCTA was used to detect and stratify coronary plaque into three categories: any plaque, significant plaque, and high-risk plaque. High-risk plaque features include low attenuation on CCTA (non-calcified plaque) and significant stenosis (arterial narrowing by 50% or more). These predict a tenfold rise in coronary event rates after five years compared to people with normal coronary arteries.
Study findings
People in the lowest DI tertile (most inflammatory) were younger and less likely to have a family history of cardiovascular events. In this lowest DI tertile, 62% were men compared to 33% in the highest tertile. They had elevated high-sensitive C-reactive protein levels, the highest cardiometabolic risk (increased blood lipids, blood pressure, diabetes), lower exercise duration, and higher odds of smoking, alcohol consumption, and total energy intake.
Coronary plaques were detected in 44.3% of people with the lowest DI compared to 36.3% of those with the highest DI, indicating a higher prevalence of plaque among those with less healthy diets. Significant stenosis (narrowing of 50% or less of the original vessel diameter) was observed in 6.0% of people in the lowest DI tertile vs. 3.7% in the highest.
Specifically for non-calcified plaques with significant stenosis, the rates were 1.5% for the lowest DI and 0.9% for the highest DI. Calcification, a higher total plaque burden, and increased odds of significant vessel narrowing were all correlated with the lowest DI tertile.
People in the lower two DI tertiles were more likely to have plaque, and the more segments involved, the more vessel narrowing to a significant degree and the more plaque calcification. In statistical models adjusted for age and sex, high-risk plaque was 67% more likely in the lowest tertile (odds ratio 1.67) compared to the highest tertile.
However, after adjusting for additional factors such as waist circumference, triglyceride levels, and hypertension, this association was attenuated and, in some cases, became non-significant.
Non-significant non-calcified stenosis was 23% more likely in the lowest tertile, while calcified non-significant stenosis was 37% more common. The right coronary and left anterior descending arteries are more often affected in people with lower DI.
A lower DI may increase the risk of coronary atherosclerosis in part due to its association with increased waist size, higher blood pressure, and elevated blood triglyceride levels. These factors account for between 21% and 57% of the differences seen in plaque characteristics with waist circumference having the largest influence.
These results confirm that CVD risk is elevated in obesity, which is more common among individuals with unhealthy dietary patterns. These, in turn, are associated with lifestyle factors like smoking, drinking, and sedentary habits.
Women with a low DI had a worse coronary plaque risk status than men. However, the stronger association in women was observed mainly for overall plaque presence, not all specific plaque types. Total caloric intake and education status influenced the DI rather than plaque presence or features. Conversely, age and sex affected plaque presence and risk status.
Both the DI and plaque-related outcomes were affected by age and sex, smoking, waist size, triglycerides, and hypertension. These factors did not correlate with each other except for a higher renal output, and lower waist size and alcohol consumption, among women compared to men.
It is important to note that dietary information was self-reported using a food frequency questionnaire, which introduces potential recall bias and uncertainty in estimating actual intake. Additionally, the study lacked detailed data on participants’ ethnicities, limiting its generalizability beyond Swedish populations.
Conclusions
This is the first extensive study to explore cardiovascular risk profiles with CCTA-based coronary assessment and self-reported dietary habits in a middle-aged population-based cohort. Its novel findings correlate a pro-inflammatory diet low in fiber and high in red meat content with an increased risk of developing high-risk coronary plaques.
The effect could be partly driven by increased waist size, higher triglyceride levels in the blood, and high blood pressure. Altered metabolic pathways and circulatory shifts thus influence the ultimate impact of the diet on coronary atherosclerosis.
While supporting earlier research findings, the current study extends them by using granular plaque phenotypes to compare outcome variability with differences in the DI. However, as an observational and cross-sectional study, it can only establish associations and not causation.
“Our findings strengthen the importance of cardioprotective dietary recommendations.”
Download your PDF copy now!