New research uncovers a striking link between endometriosis and autoimmune conditions, suggesting a shared biological mechanism and opening the door to earlier diagnosis and targeted treatment.
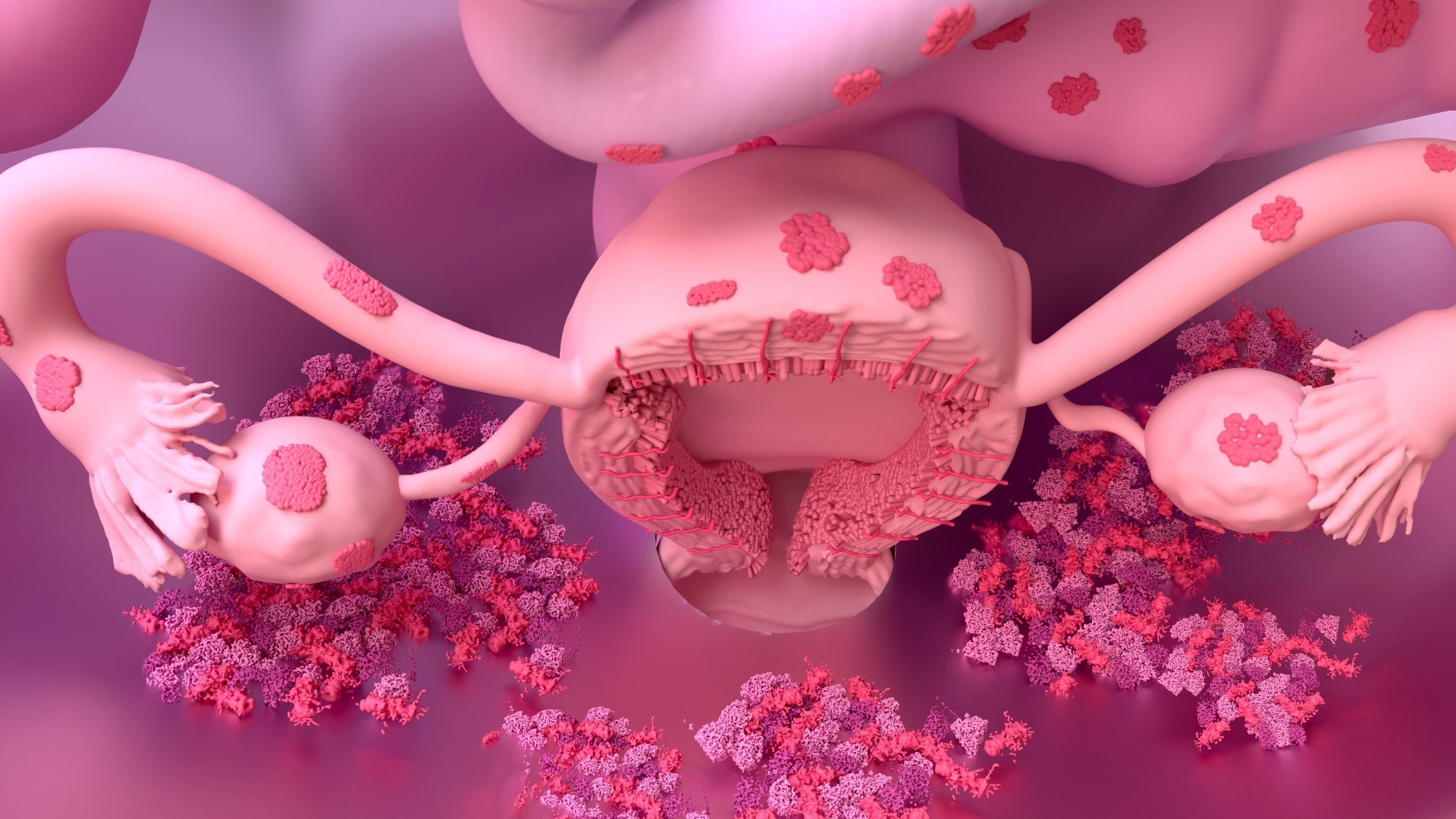 Study: Endometriosis and autoimmunity: a large-scale case-control study of endometriosis and 10 distinct autoimmune diseases. Image credit: Design_Cells/Shutterstock.com
Study: Endometriosis and autoimmunity: a large-scale case-control study of endometriosis and 10 distinct autoimmune diseases. Image credit: Design_Cells/Shutterstock.com
A recent study in NPJ Women’s Health examined two large databases of women, matching women with endometriosis to controls. The results show that endometriosis is associated with a greater risk of newly diagnosed autoimmune disease within two years.
Introduction
Endometriosis is a systemic inflammatory disease that can cause chronic, sometimes disabling, pain and infertility among women. It can be a painful condition, affecting 10% of women, in which they have tissue closely resembling uterine endometrium is found outside the uterine cavity. Autoimmune diseases result from attacks by the body’s immune system on its healthy tissue, affecting about 8% of people. Women account for 80% of autoimmune disease victims.
Both endometriosis and autoimmune conditions are inflammatory and share several clinical features. In addition, both severely reduce quality of life. These common characteristics have led to the idea that they are related, further strengthened by their observed association.
Immune cell defects and elevated inflammatory mediators characterize both endometriosis and autoimmune disease. Although genetic correlations between endometriosis and autoimmune conditions like rheumatoid arthritis and multiple sclerosis have shown mixed results, recent studies indicate potential positive genetic associations.
Shared underlying pathways may explain the association between these conditions. For instance, endometriosis lesions trigger inflammation, leading to adhesions and scar formation. These further elevate the release of inflammatory mediators like interleukins and prostaglandins, contributing to autoimmune disease processes.
Immune cell activation is altered in women with endometriosis, as suggested by higher numbers of peritoneal macrophages and neutrophils, reduced killer cell activation, and aberrant T cell function. Age and differences in social status, environmental exposures, and lifestyle affect the risk of systemic inflammation.
Conversely, the inflammation associated with autoimmune conditions could predispose to endometriosis. These could explain the varying risk of autoimmune disease among endometriosis patients in different studies.
Knowing how soon autoimmune disease was diagnosed after an endometriosis diagnosis might support the existence of common pathogenetic mechanisms. The current study explored associations detected within a defined window of time, as opposed to ever occurring during the patient's lifespan, from large cohorts of routine care rather than experimental interventions.
The study also noted that delays in diagnosing endometriosis and autoimmune diseases may distort the apparent order of onset, highlighting the challenge of determining which condition truly appears first.
Study findings
The data came from two studies, including 332,409 women with endometriosis and 1,220,932 controls. The authors used two large-scale administrative claims databases, commercial insurance and Medicaid databases, to ensure broad population coverage and generalizability. About 5% of women with endometriosis were diagnosed with one or more autoimmune conditions within two years, vs. 1.4% of controls.
The odds of diagnosing several autoimmune diseases within two years were two- to threefold higher among endometriosis patients compared to the control group. These included rheumatoid arthritis, Hashimoto’s disease, pernicious anemia, systemic lupus erythematosus, and multiple sclerosis.
The odds were modestly increased for type 1 diabetes mellitus and Graves’ disease. However, the odds of Sjögren’s syndrome and myositis were up to sixfold higher for some cohorts compared to controls.
Overall, the odds of being diagnosed with an autoimmune disease were twofold higher among endometriosis patients than controls. At three years, the associations with type 1 diabetes were no longer statistically significant.
The study does not establish causal associations. Associations between endometriosis and autoimmune disease could be due in part to the fact that both are characterized by chronic systemic inflammation, and both affect multiple organs and systems throughout the body. Chronic inflammation in endometriosis may elevate the risk of autoimmune reactions, with synergism between genetic tendencies and inflammation.
Alternatively, physicians may identify other conditions, including autoimmune disease, when investigating the signs and symptoms of endometriosis, accounting for their association.
A third hypothesis backed by emerging evidence is that the presence of autoimmune disease might predict more advanced endometriosis. That is, endometriosis remains undiagnosed in many women until the onset of autoimmune disease with symptoms that cannot be ignored. During the investigation of the latter, late-stage endometriosis comes to light.
However, this study only included women with diagnosed endometriosis. Possibly, they had worse symptoms because of accompanying autoimmune disease and endometriosis. Thus, the finding of comorbid autoimmune disease might be due to greater symptom severity rather than a shared biological mechanism.
Additionally, since the study relied on administrative claim data, the findings may reflect diagnostic coding practice or healthcare utilization patterns rather than purely biological links.
Notably, the researchers used validated phenotype definitions for endometriosis and autoimmune diseases and applied Bonferroni corrections to account for multiple comparisons, strengthening the statistical reliability of results. Confounding factors need to be adjusted for when conducting future research.
Conclusions
For the first time, this study demonstrated that patients with endometriosis were at twofold risk of being diagnosed with one or more autoimmune diseases within two years of the initial diagnosis, compared to controls.
This provides more evidence in favor of such an association and suggests the existence of common biological pathways that require further exploration. Earlier diagnosis of endometriosis and autoimmune conditions might help to determine their common origins by tracking their onset. Coupled with mechanistic research, this could help uncover the pathogenesis of these conditions.
The study also emphasized the need for future work using more granular clinical data sources and longitudinal follow-up to account for confounders and diagnostic lags.
Download your PDF copy now!
Journal reference:
- Aziz, M., Beaton, M. A., Aziz, M., A., et al. (2025). Endometriosis and autoimmunity: a large-scale case-control study of endometriosis and 10 distinct autoimmune diseases. NPJ Women’s Health. Doi: https://doi.org/10.1038/s44294-025-00086-8. https://www.nature.com/articles/s44294-025-00086-8