Scientists uncover how shifts in gut fungi, shaped by genes and diet, may influence disease severity in people with multiple sclerosis, paving the way for new microbiome-based treatments.
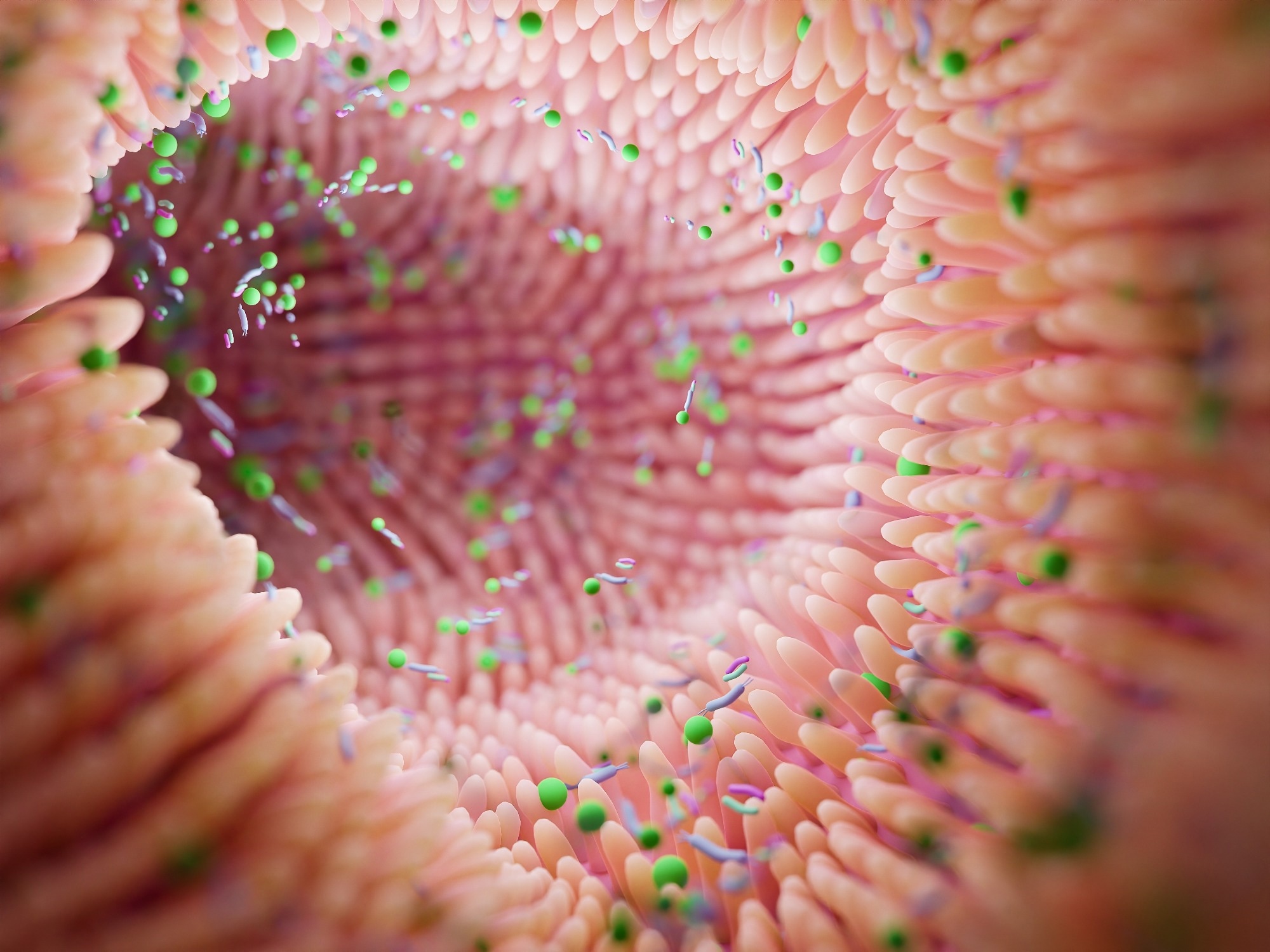 Study: Exploring the mycobiota in multiple sclerosis: its influence on disease development and progression. Image credit: Troyan/Shutterstock.com
Study: Exploring the mycobiota in multiple sclerosis: its influence on disease development and progression. Image credit: Troyan/Shutterstock.com
A new study published in Frontiers in Immunology revealed that the fungal component of human gut microbiota is associated with and may influence the development and progression of multiple sclerosis, a chronic autoimmune disease of the central nervous system.
Background
Multiple sclerosis (MS) is a progressive neurodegenerative disease that develops when the body’s immune system mistakenly attacks the protective covering of nerve fibers (myelin sheath) in the brain. This leads to inflammation, nerve damage, and disrupted communication between the brain and the rest of the body.
Genetic, environmental, and lifestyle factors contribute significantly to the development and progression of MS. Recent evidence also links the immune-modulatory role of human gut microbiota with MS pathogenesis. Although most studies have particularly investigated the role of the gut bacterial community in MS, some recent evidence has highlighted the involvement of the gut fungal community (mycobiota).
In patients with MS, an increased abundance of antibodies specific to Candida albicans has been observed. Candida albicans is the most common fungal member of the gut microbiota, mostly harmless when present in low abundance. The specific enzyme activity of Candida albicans has also been correlated with disease severity.
Given the potential involvement of mycobiota in MS pathogenesis, the current study investigated the composition of the gut mycobiota in MS patients across different treatment conditions and disease stages. The primary aim was to decode potential associations between gut fungal communities, immune function, and genetic risk factors in MS.
The study
The study involved 50 patients with MS and 25 healthy individuals as controls. Fecal and blood samples were collected from participants for the mycobiota characterization and risk factor analysis.
Two inflammatory risk factors, calprotectin and chitotriosidase, and the strongest genetic risk factor, the HLA-DRB1*15 variant, were analyzed. Chitotriosidase, an important biomarker of MS, has been linked to fungi in the cerebrospinal fluid derived from MS patients. Calprotectin is another important biomarker with strong antimicrobial activity against fungi.
The HLA-DRB1*15 gene variant is the most substantial risk factor for MS, playing a critical role in regulating T cell-mediated and antibody-mediated immune responses. The specific variants HLA-DRB1*1501 and HLA-DRB1*1503, which confer the most significant predisposition to MS, have been linked to an increased incidence of fungal infections.
The participants also completed a food frequency questionnaire to assess the impact of dietary components on fungal populations.
Key findings
The study findings revealed a trend toward greater fungal abundance and diversity in MS patients compared to healthy individuals, although differences were not statistically significant for overall diversity measures. Specific fungal genera, including Saccharomyces, Torulaspora, and Malassezia, showed notable patterns in the dataset. Still, Torulaspora and Debaryomyces were more characteristic of untreated MS patients, while Saccharomyces was more typical of controls.
The study found a strong association between the mycobiota profile of MS patients and the MS genetic risk factor HLA-DRB1*15 variants, with carriers of the HLA-DRB1*1501 variant exhibiting a higher risk of developing severe MS. Specifically, patients carrying the HLA-DRB1*1501 variant had higher abundances of the Debaryomyces and Talaromyces genera. In contrast, non-carriers exhibited higher abundances of the genus Cladosporium.
Regarding MS biomarkers, the study found disease-specific correlations between some fungal groups and blood levels of calprotectin and chitotriosidase, but group-level biomarker differences were generally insignificant. For example, chitotriosidase levels increased with age in MS patients. They tended to be higher in untreated patients with a worse prognosis, while calprotectin levels were found to influence mycobiota composition but did not significantly differ between patients and controls.
Regarding the impact of dietary habits, the study found significantly higher cholesterol consumption in MS patients compared to that in healthy individuals. This increased cholesterol intake was associated with distinct changes in gut mycobiota composition, highlighting altered lipid metabolism in MS.
Study significance
The study provides new insights into the changes in gut fungal populations that may accompany MS pathogenesis and progression. The findings about associations between fungal biomarkers, genetic risk factors, and dietary habits would help better understand MS pathogenesis and support the development of potential mycobiota-targeted therapy.
The study identified Malassezia as a fungal genus correlated with greater MS severity and disability, though overall mycobiome diversity (Shannon index) predicted severity more strongly than any single genus. Malassezia has a high affinity for lipids in the brain, together with immune suppression and blood-brain barrier disruption in MS, which may facilitate the entry of Malassezia into the brain and subsequent disease progression.
Overall, the study findings on significant associations between specific fungal populations and disease severity highlight the importance of considering gut fungal dynamics in MS pathology. Since the fungal and bacterial populations are closely interconnected, and changes in one population can reciprocally influence the other, it is vital to consider the entire gut microbiota as an integrated ecosystem rather than focusing on a single kingdom to better understand MS pathogenesis.
This study sets the groundwork for the systematic characterization of minority microbial communities, such as fungi, within the broader microbiome landscape, highlighting the potential role of gut mycobiota as a biomarker or therapeutic target in future MS research rather than as an established causal factor.
Download your PDF copy now!