Scientists find fat-derived particles could accelerate Alzheimer’s, connecting obesity to toxic brain changes.
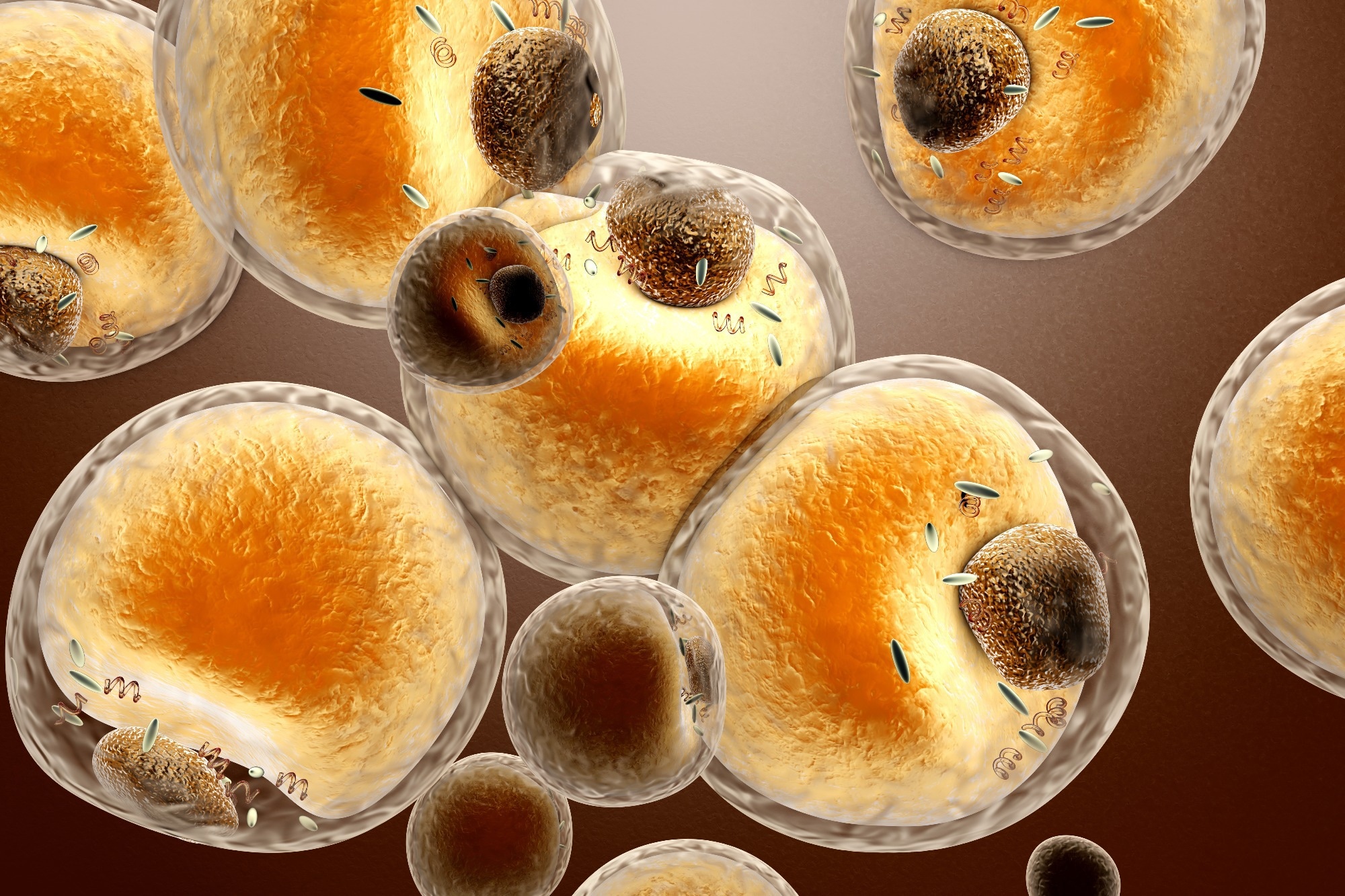 Study: Decoding adipose-brain crosstalk: Distinct lipid cargo in human adipose-derived extracellular vesicles modulates amyloid aggregation in Alzheimer's disease. Image Credit: Spectral-Design / Shutterstock.com
Study: Decoding adipose-brain crosstalk: Distinct lipid cargo in human adipose-derived extracellular vesicles modulates amyloid aggregation in Alzheimer's disease. Image Credit: Spectral-Design / Shutterstock.com
Alzheimer’s disease (AD) could affect 82 million people by 2050. The brain is rich in fats, which comprise a significant portion of the myelin sheath and neuronal membranes. Disruptions in lipid metabolism—whether due to genetic factors or environmental influences—can increase the risk of AD, particularly when linked to obesity.
In a recent study published in Alzheimer’s & Dementia, researchers discuss the role of extracellular vesicles as a potential link between obesity and Alzheimer’s disease (AD).
How fat dysregulation leads to amyloid pathology
During obesity, lipotoxicity, which reflects abnormally high lipid levels, can damage brain tissue by causing inflammation. This condition is worsened by the presence of adipokines, which are chemicals released from fat tissue that activate immune-inflammatory pathways.
According to the amyloid cascade hypothesis, neurodegeneration in AD begins with the formation of the amyloid-β (Aβ) 40 and 42 peptides. Following their secretion into the extracellular space, these peptides aggregate under certain conditions to form small oligomers or fibrils.
Aβ fibrillization, the process by which Aβ fibrils are generated, precedes amyloid plaque formation, a characteristic feature of AD brains. Plaques are lipid-enriched and can be produced during fat-dependent Aβ peptide condensation, which leads to brain inflammation, neuronal injury, inadequate energy supply, and oxidative stress.
Extracellular vesicles (EVs) from fat cells are membrane-bound molecules that contain fat released from different regions throughout the body. Often originating from peripheral fat tissue, these EVs may cross the blood-brain barrier to change the balance of fats in the brain, which increases the risk of neurodegenerative disease.
Aβ fibrilization is affected by genetic and environmental factors, including lipid-laden EVs from peripheral fatty tissue.
The current study's researchers removed and purified EVs, mostly exosomes, from subcutaneous and visceral fat samples obtained from lean and obese people. In addition to quantifying the complete array of fat molecules present in these EVs, in vitro Aβ aggregation was quantified using purified Aβ40 and Aβ42 peptides in fat-rich environments that resemble the brain milieu in health and disease.
Study findings
EVs obtained from obese individuals were characterized by a distinctive lipid profile that reflects their role as fat carriers originating from subcutaneous and visceral fat tissues. Purified EVs isolated from obese people had higher concentrations of lysophosphatidylcholine (LPC) and sphingomyelin (SM), which suggests abnormal fat metabolism.
Both saturated and unsaturated fatty acids were directly implicated in Aβ fibrilization when present at lipotoxic concentrations, with LPC18:0 lipids exhibiting particularly strong aggregation effects. Notably, low levels of some sphingomyelins like SM23:0 reduced Aβ aggregation, whereas higher concentrations of this sphingomyelin led to increased Aβ aggregation.
SM16:0 and SM18:0 also promoted Aβ aggregation, the latter of which is the most abundant sphingomyelin species present in the brain. High levels of LPC18:0 also correlated with a marked increase in Aβ42 fibrilization.
Palmitic acid, the most abundant saturated fatty acid present in the human body, did not significantly affect Aβ aggregation under normal conditions. However, pathologically high levels of palmitic acid led to increased Aβ fibrilization.
These findings provide compelling molecular evidence linking peripheral lipid imbalance to Aβ aggregation, suggesting that metabolic dysfunction associated with obesity may contribute to central amyloid pathology via adipose-derived EV lipids.”
Study limitations
The study findings suggest that adipose-derived EVs can directly interfere with amyloid aggregation kinetics in the brain microenvironment, increasing the risk of neurodegenerative diseases like AD. Nevertheless, additional research, including in vivo studies, longitudinal clinical cohorts, and direct measurement of brain amyloid pathology, must be conducted to confirm whether these lipid-based EVs contribute to the development and progression of AD.
Click here to download a PDF copy of this page
Journal reference:
- Yang, L., Chan, M., Sheng, J., et al. (2025). Decoding adipose–brain crosstalk: Distinct lipid cargo in human adipose-derived extracellular vesicles modulates amyloid aggregation in Alzheimer's disease. Alzheimer’s & Dementia. doi:10.1002/alz.70603.