Most scientists believe that SARS-CoV-2 acquires mutations slower than other RNA viruses. The researchers in the current study argue that this has not been empirically verified. Instead, the mutation burden and rate at which new mutations develop – about 1x10-3 substitutions per base per year – is estimated only for a situation in which neutral genetic drift is expected and not when any positive selection pressure was operating, such as population immunity.
It is now known that the rapid transmissibility of the virus precludes the development of adaptive humoral immunity in the host before it spreads to the next individual, since the former occurs within about 10 days, but peak spread occurs around the time when the earliest symptoms set in. As a result, the virus is hardly exposed to antibodies before it is transmitted, explaining why viral genomic sequences show little evidence of positive selection.
At the current rate of viral evolution, the virus is likely to evade the neutralizing antibodies being used to prevent the infection in the form of convalescent plasma. Therefore, under this type of positive selection pressure, antibody-evading viral mutants are likely to arise rapidly, enabling second and successive waves of infection.
Two factors determine the rate of adaptation of the virus: the rate of mutation and mutational tolerance. Mutation rates are important only if they allow the virus to escape from antibody-mediated neutralization by modifying the neutralizing epitopes, without impacting viral infectivity. Thus, high mutation rates must coexist with the ability of antigens to evolve successfully so as to evade the immune response without impacting viral fitness. Antigenic evolvability is favored by natural selection.
Evolutionary cost of RBD-immune evading mutations
The researchers found three clusters of epitopes on the receptor-binding domain (RBD) of SARS-CoV-2, with the largest showing significant overlap with the angiotensin-converting enzyme 2 (ACE2) binding surface. Some parts of the RBD are independently targeted by natural human antibodies in different individuals, showing a narrow range of epitopes targeted by these antibodies. If these important epitopes are modified by mutation, the virus could escape from inhibition by several neutralizing antibodies.
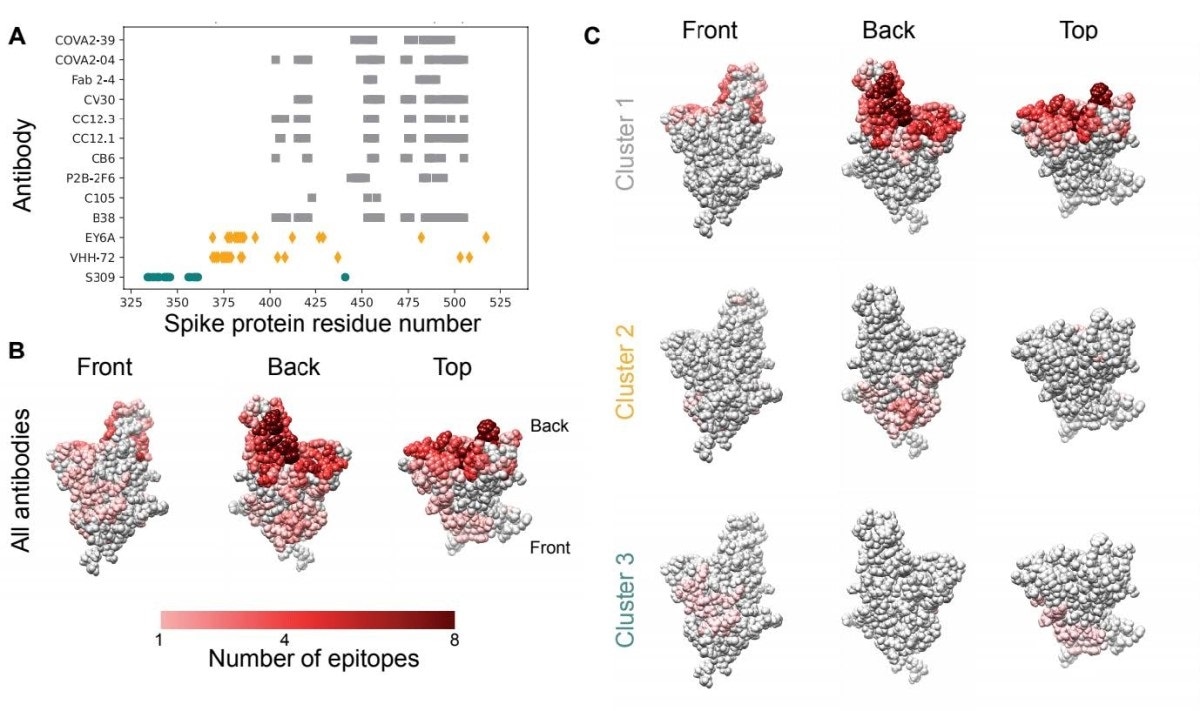
Epitopes for antibodies targeting the spike protein RBD overlap substantially. A. Contact residues for spike protein RBD antibody epitopes. Colors and symbols denote antibody clusters: grey squares: cluster 1, yellow diamonds: cluster 2, green circles: cluster 3. B. RBD structure with each residue colored by the number of antibody epitopes including it, compiled from PDB data. C. RBD structure, colored by the number of antibody epitopes that each residue is part of, by epitope cluster.
Analysis of available sequences shows that 23 of 32 naturally occurring mutations in circulating SARS-CoV-2 strains are associated with in vitro resistance, and are therefore able to escape mutations. However, they do not inhibit spike-ACE2 binding, or even increase it. They also leave viral RBD expression unchanged. The researchers say these findings suggest that "the optimal escape pathways for these antibodies may not reduce cellular infectivity or viral fitness."
Early emergence of immune-evading mutants
The researchers predicted the frequency of these escape mutants in the population before and after prophylactic antibodies began to be widely used. In the earlier case, the escape mutations offer no benefit in terms of transmission, but may somewhat reduce viral fitness in terms of decreased ACE2 binding affinity, or other negative factors. This agrees with observations that indicate a weak negative selection for this virus, with the weeding out of deleterious variants.
The constant generation of new mutants by de novo mutation allows them to be present in the population despite their reduced fitness. But once the population contains a significant number of neutralizing antibodies, these resistant mutants will be beneficial, and will be positively selected if their frequency is high enough. In that situation, the use of one or two NAbs will no longer effectively counter the virus.
Mathematical modeling suggests that each NAb is inhibited by one or more single nucleotide changes. With an estimated mutation rate of 1x10-5 to 1x10-4 per base per transmission, and with multiple point mutations capable of evading one NAb, the per transmission mutation rate for an evading mutation for one antibody in particular may be an order of magnitude greater than the per-base mutation rate, or even more.
With the expected number of infected individuals with viral strains containing one or two evading point mutations being over 10,000 worldwide, over a range of fitness losses, the researchers say, "This number far exceeds the number of individuals required to exceed the boundary at which natural selection and not drift is the primary driver of evolution."
If the fitness advantage is 0.1, it is equivalent to administering an effective preventive NAb to 14% of the population. In this scenario, the immune escape mutant will be positively selected and overtake the wild-type virus if 10 or more people are harboring the escape mutant. This is adequate to eventually result in widespread NAb resistance, making the use of prophylactic antibodies ineffectual.
If an antibody cocktail is used, however, more than one nucleotide change could be required for resistance. For instance, if two specific mutations in combination are required for the individual to be resistant to the antibody mixture, the expected number of infected individuals who contain the virus capable of immune evasion is much lower, by orders of magnitude. Thus, in the current situation, with more than 50 million infections being quite possible, it is probable that there are hundreds of such individuals.
If a triple mutant is considered, the fitness cost would have to be less than 0.4 to reach appreciable frequencies in the population. If the number of required mutations is higher than this, they are not expected to reach such frequencies unless the fitness cost is extremely low. Thus, if triple or higher mutations are required, population-level resistance to NAbs is unlikely, conclude the scientists.
Can mutants establish themselves?
If prophylactic single and double NAbs are used, escape mutants will be spontaneously generated and positive selection pressure will ensure that they are established. This involves transiting through a region of intermediate lower fitness variants lacking one or more, but not all, the required mutations.
The benefit of the combination for viral transmission decides how fast these mutants are established at the population level. This advantage will only increase as the NAb prophylactic is more widely used. While double mutants conferring antibody resistance are expected to be established in a few months if about 40 million infections are present, triple and higher mutants will take much longer despite the widespread use of such prophylactics with strong selection pressure and under a range of fitness costs.
The higher the rate of mutation, the shorter the interval for population-level resistance. The researchers comment, "Anticipating the virus' counter-move to the widespread deployment of spike RBD-targeting nAbs has significant implications for our ability to prevent spread of the disease via an antibody based prophylactic strategy."
This type of selective establishment of one strain has already been observed, with the D614G mutation rising to dominance shortly after its introduction into various regions of the world. Within 6 months, it accounted for almost 8 in 10 isolates worldwide, which was attributed to its increased infectivity and the fact that it arose readily in a large number of infected individuals. At present, another mutant, the 2A.EU1 variant appears to be taking over.
Selection pressures can allow antibody-evading mutations to expand and disarm antibody-based prophylactics. To counter this, the study suggests combinations of NAbs should be used to engage 3 or more distinct non-overlapping epitopes, preferably including those outside the three clusters mentioned to exist on the RBD itself. If the NAbs are from the same cluster, their epitopes must not overlap.
The scientists predict that with a wider use of more effective individual NAbs, resistance will emerge more rapidly. Again, the use of NAbs must be tailored since this tool's effectiveness depends on using multiple antibody combinations, which use multiple epitopes and require different mutations to escape their effects and the extent of overlap between their mutations.
The researchers summarize: "SARS-CoV-2 will evolve quickly to evade widely deployed spike RBD-targeting monoclonal antibodies, requiring combinations with at least three antibodies to suppress viral immune evasion."
Future work should explore the role of cellular immunity escape mutations as well, in the RBD as well as other viral proteins. The question of SARS-CoV-2 quasispecies is also important in that the diversity within an individual host is perhaps adequate to allow the emergence of resistance to therapeutic NAbs as well.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources