Can coronavirus disease 2019 (COVID-19) affect the eye? New research suggests the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) can enter the eye and infect photoreceptor and retinal ganglion cells. In addition, SARS-CoV-2 infection increases the expression of several inflammatory genes, including the cytokine interleukin 33 (IL33), which is linked to COVID-19 disease and retinal degeneration.
Antibodies blocking the ACE2 receptor reduce infection of retinal cells, suggesting SARS-CoV-2 infection works in an ACE2-dependent manner.
The study “SARS-CoV-2 infects and replicates in photoreceptor and retinal ganglion cells of human retinal organoids” is published on the preprint bioRxiv* server.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Researchers find evidence of SARS-CoV-2 in the human retina
The researchers exposed mature retinal organoids to SARS-CoV-2 and then incubated the organoids for different lengths of time to observe the virus’s infection and replication rate.
SARS-CoV-2 did infect retinal cells, as confirmed by a PCR test. A viral plaque assay detected viral plaques in retinal cells infected with SARS-CoV-2, suggesting SARS-CoV-2 successfully replicated in human retinal tissue.
Viral titers increased after 48 hours. However, titer levels reverted after three days.
Immunofluorescence captured the presence of SARS-CoV-2 nucleocapsid protein-positive cells in the retinal organoids.
Cells infected by SARS-CoV-2 appeared to affect mature retinal organoids compared to younger retinal organoids. In mature organoids, SARS-CoV-2 was more likely to affect the outer retina. Younger retinal organoids were infected from SARS-CoV-2 in the inner retina.
SARS-CoV-2 infects mature retinal ganglion cells and photoreceptors
The findings suggest various cells in the retina are susceptible to SARS-CoV-2 infection.
The cells more likely to become infected by SARS-CoV-2 were retinal ganglion cells.
In smaller numbers, OTX2+ photoreceptors, few bipolar cells, and AP2A+ amacrine cells tested positive for SARS-CoV-2’s nucleocapsid protein. There were even fewer VSX2+ progenitor cells infected by SARS-CoV-2.
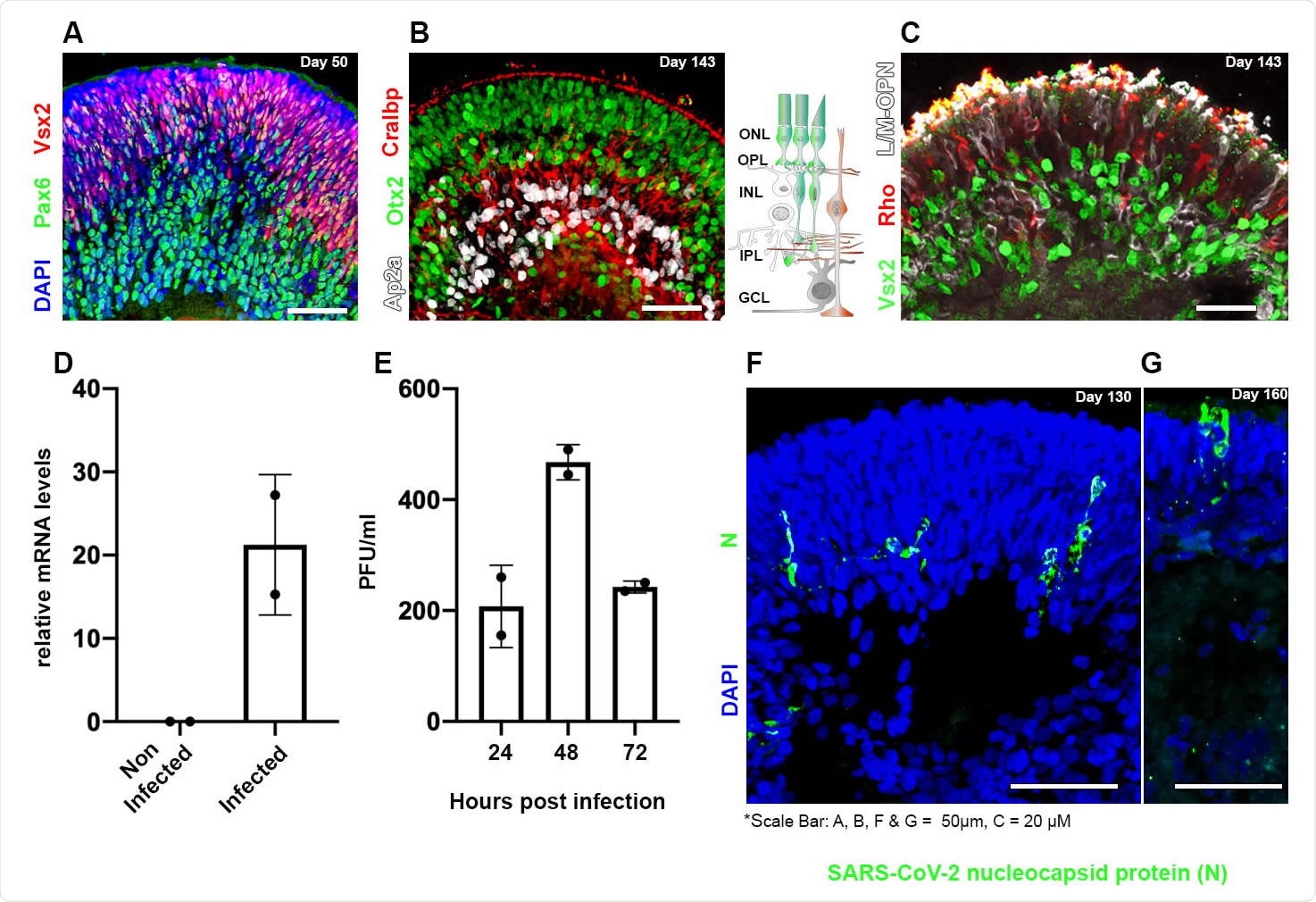
Human iPSC-derived retinal organoids can be infected by SARS-CoV-2 Retinal organoids on day 50 of differentiation are shown to contain VSX2+ (green) retinal progenitors and PAX6+ (white)/VSX2- amacrine and retinal ganglion cells (RGCs) (A). On day 143 of differentiation, the organoids are shown to be organized in a layered structure and to contain AP2a+ (white) amacrine and horizontal cells, CRALBP+ (red) Müller glia cells, and OTX2+ (green) cells (B). The sketch in (B) depicts the cell types and structure of the vertebrate retina. ONL: outer nuclear layer; OPL: outer plexiform layer; INL: inner nuclear layer; IPL: inner plexiform layer; GCL: ganglion cell layer. On day 143 of differentiation, the photoreceptors in the organoids are stained against the photosensitive proteins L/M-OPN (white) and RHODOPSIN (RHO, red) (C). Real-time PCR identified SARS-CoV-2 genomic RNA within retinal organoids treated with SARS-CoV-2 but not in controls on day 125 (D). A viral plaque assay was used to assess viral titrations in SARS-CoV-2 treated organoids on day 125 (E). Each repeat (N=2) in (D) and (E), is a separate group of five organoids infected or not infected in a separate well. Immunofluorescence analysis was used to detect SARSCoV-2 nucleocapsid (N)-positive cells in infected organoids at day 130 (F) or 160 (G) of differentiation.
SARS-CoV-2 increases the expression of genes related to inflammation
An upregulation of 366 genes and a downregulation of 393 genes was observed in the study.
“The top five most enriched biological process categories in this analysis were “Potassium ion transport,” “Cellular response to cytokine stimulus,” “Cellular response to BMP stimulus,” “Metal ion transport,” and “Cytokine-mediated signaling pathway,” explained the researchers.
An increase in cytokine-related gene expression suggests an immune response in reaction to the SARS-CoV-2 virus.
Genes related to the JAK-STAT signaling pathway — pathway involved in inflammation and an innate antiviral interferon response — were also enriched after SARS-CoV-2 infection.
The researchers suggest the upregulation of potassium ion transport-related genes may be linked to the low potassium levels observed during COVID-19 illness.
Additionally, SARS-CoV-2 appears to increase IL33 gene expression as it was the most upregulated cytokine in all infected retinal organoids. IL33 is implicated in retinal inflammation and photoreceptor degradation.
NLRP1 is another upregulated inflammatory gene observed during SARS-CoV-2 infection. In addition, the gene is associated with retinal ganglion cell death during acute glaucoma.
SARS-CoV-2, similar to other coronaviruses, may negatively impact the cell cycle and the DNA damage response. Downregulation of genes involved in DNA metabolism, repair, and recombination was observed in retinal organoids after infection.
Blocking ACE2 receptor reduces SARS-CoV-2 infection
ACE2 mRNA levels are low in the human retina. However, ACE2 protein is abundant.
SARS-CoV-2 infection did not change ACE2 expression, indicating a lack of ACE2 upregulation in retinal cells.
When researchers treated infected retinoids with an anti-ACE2 antibody, the number of SARS-CoV-2 nucleocapsid proteins in infected cells significantly decreased.
Based on the results, the researchers conclude SARS-CoV-2 infection and replication in retinal cells are dependent on ACE2 receptors.
Drugs targeting ACE2 receptors may help in treating COVID-19 patients with retinal symptoms.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Menuchin-Lasowski et al. (2021). SARS-CoV-2 infects and replicates in photoreceptor and retinal ganglion cells of human retinal organoids. bioRxiv. Doi: https://doi.org/10.1101/2021.10.09.463766, https://www.biorxiv.org/content/10.1101/2021.10.09.463766v1
- Peer reviewed and published scientific report.
Menuchin-Lasowski, Yotam, André Schreiber, Aarón Lecanda, Angeles Mecate-Zambrano, Linda Brunotte, Olympia E. Psathaki, Stephan Ludwig, Thomas Rauen, and Hans R. Schöler. 2022. “SARS-CoV-2 Infects and Replicates in Photoreceptor and Retinal Ganglion Cells of Human Retinal Organoids.” Stem Cell Reports 17 (4): 789–803. https://doi.org/10.1016/j.stemcr.2022.02.015. https://www.cell.com/stem-cell-reports/fulltext/S2213-6711(22)00104-7.