According to the World Health Organization (WHO), coronavirus disease 2019 (COVID-19), which is caused by infection with the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is associated with an increased risk of intensive care (ICU) admission during pregnancy. SARS-CoV-2 infection in the mother also predisposes her to preterm birth and increases the likelihood that the infant will require neonatal care after birth.
The SARS-CoV-2 Omicron (B.1.1.529) variant of concern (VOC) was first reported in the United Kingdom (UK) in November 2021. With the SARS-CoV-2 Alpha and Delta VOCs, severe maternal infection was more common as compared to those infected with the wild-type strain. Meanwhile, non-pregnant women who contracted Omicron infection had a reduced likelihood of severe pulmonary disease than those with the Delta infection.

Study: Severity of maternal SARS-CoV-2 infection and perinatal outcomes during the Omicron variant dominant period: UK Obstetric Surveillance System national cohort study. Image Credit: christinarosepix / Shutterstock.com

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
About the study
In a recent study published on the medRxiv* preprint server, researchers describe the characteristics of pregnant women hospitalized due to COVID-19. These characteristics include vaccination status, the severity of symptoms, management protocols, pregnancy status, and perinatal outcomes during the initial period of Omicron dominance in the U.K.
This was a national and prospective observational cohort study that utilized the U.K. Obstetric Surveillance System (UKOSS), which provides data from all U.K. hospitals with a consultant-led maternity unit. Women hospitalized during pregnancy with a positive SARS-CoV-2 polymerase chain reaction (PCR) test during admission were included in the current study.
Study participants were categorized into either a symptomatic or asymptomatic group. The symptomatic group consisted of women admitted due to COVID-19 symptoms, whereas the asymptomatic group consisted of women who were admitted for labor, obstetric care, or other reasons and were not experiencing SARS-CoV-2-related symptoms.
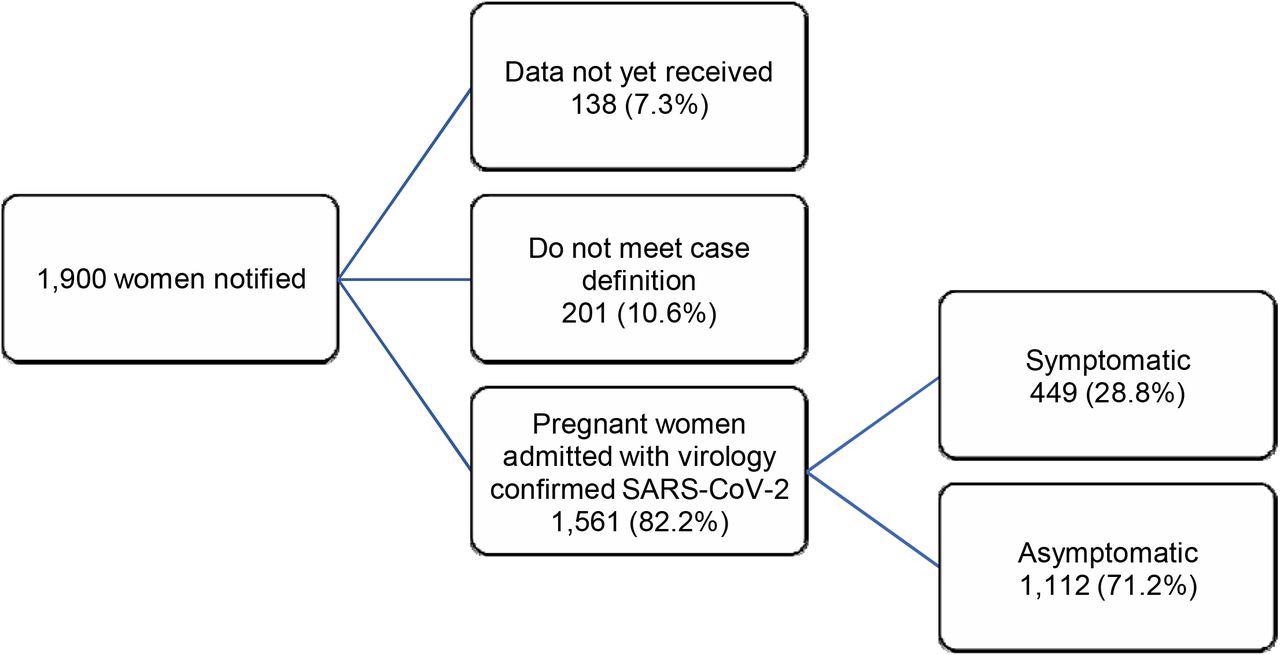
Inclusion flow chart: pregnant women admitted to hospital with SARS-CoV-2 infection, by admission group, UK, 15th December 2021 to 14th January 2022
Study findings
Overall, 1,561 women with confirmed COVID-19 positive tests were admitted during the study period of December 2021 to January 2022. Among these, 28.8% were symptomatic.
The symptomatic group had a slightly higher proportion of women with a body mass index (BMI) of 30kg/m2 or above. Notably, this group had a lower percentage of women who reported Black, Asian, or other minority backgrounds.
The symptomatic group included 50.8% women with gestational age ranging from 22-36 weeks, whereas the asymptomatic group had 22.8% women belonging to this gestational age range. The vaccination status of 1,274 women in the symptomatic group was known as compared to 891 women in the asymptomatic group.
It was also noted that two asymptomatic women required ICU admission for other ailments/symptoms that were not linked to COVID-19. Eighty-six symptomatic women exhibited at least one sign of moderate to severe infection; however, most of the patients in this group did not receive specific pharmacological therapy. The treatment modalities included antivirals, tocilizumab, corticosteroids, and monoclonal antibodies.
In the symptomatic group, 65.1% of women did not receive COVID-19 vaccination, 11.8% had received one vaccination dose, 19.8% had completed two vaccination doses, and 3.4% had also received a third booster dose.
In the symptomatic cohort with known vaccination status, 20.4% had moderate to severe infection. The same was true for over 20% of unvaccinated women, as well 22.2% of those who had received one COVID-19 vaccine dose.
Among women who had received two vaccination doses, 10% presented with moderate to severe infection. None of the women who were given a third vaccination dose were reported to have acquired the infection.
In the two-dose group, 40 women received their second vaccination dose more than three months before hospitalization. This cohort also included five of the nine participants who exhibited signs of moderate to severe infection. All women in the known vaccination status group who presented with signs of moderate to severe infection had incomplete vaccination statuses.
One-third of symptomatic women were discharged while still pregnant. Overall, 17.8% of births occurred within the gestational age range of 22-36 weeks in the symptomatic group, while the proportion was 10.7% in the asymptomatic group. In the symptomatic group, 7.6% were premature deliveries, none of whom were born to mothers who had completed three vaccine doses.
Overall, ten stillbirths occurred, with proportions of 0.8% and 0.9% in the symptomatic and asymptomatic groups, respectively. Among these, eight stillbirths were reported in the unvaccinated group and one vaccine-dose group.
Nonetheless, the role of SARS-CoV-2 in causing stillbirth remains unclear. In addition, 15.4% of the infants born to symptomatic women and 8.5% born to asymptomatic women required admission to the neonatal unit.
Conclusions
Taken together, the current study found that the risk of severe COVID-19 disease with the Omicron variant among unvaccinated pregnant women in the U.K. is similar to that observed during the initial wildtype SARS-CoV-2 variant dominance.
This study emphasized that in most pregnant women with SARS-CoV-2 infection, respiratory failure is preventable; however, vaccine uptake during pregnancy remains low. Thus, sincere efforts for enhanced awareness to improve vaccine uptake during pregnancy are warranted.
Rapid implementation of complete vaccination is needed in both high and low-resource settings due to the expected rise in the number of COVID-19 cases during the Omicron wave.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Engjom, H. M., Ramakrishnan, R., Vousden, N., et al. (2022). Severity of maternal SARS-CoV-2 infection and perinatal outcomes during the Omicron variant dominant period: UK Obstetric Surveillance System national cohort study. medRxiv. doi:10.1101/2022.03.07.22271699. https://www.medrxiv.org/content/10.1101/2022.03.07.22271699v1.
- Peer reviewed and published scientific report.
Engjom, Hilde M., Rema Ramakrishnan, Nicola Vousden, Kathryn Bunch, Eddie Morris, Nigel A. B. Simpson, Chris Gale, et al. 2022. “Severity of Maternal SARS-CoV-2 Infection and Perinatal Outcomes of Women Admitted to Hospital during the Omicron Variant Dominant Period Using UK Obstetric Surveillance System Data: Prospective, National Cohort Study.” BMJ Medicine 1 (1). https://doi.org/10.1136/bmjmed-2022-000190. https://bmjmedicine.bmj.com/content/1/1/e000190.