Researchers engineered an injectable silica-based scaffold that trains the immune system to attack S. aureus on medical implants, cutting bacterial load dramatically and even clearing infection entirely in some animals.
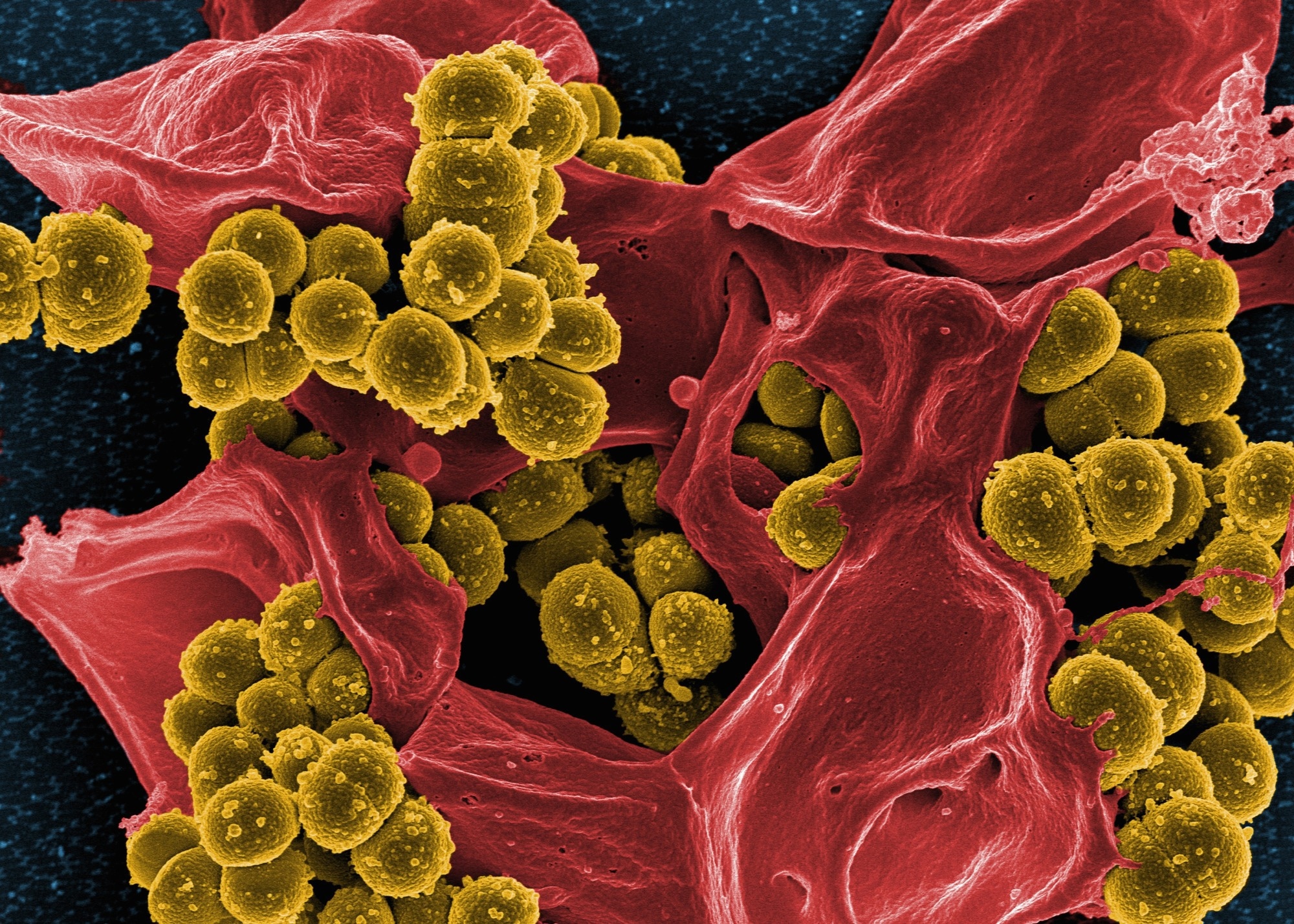 Study: Scaffold vaccination for prevention of orthopedic device infection. Image credit: Connect Images - Curated/Shutterstock.com
Study: Scaffold vaccination for prevention of orthopedic device infection. Image credit: Connect Images - Curated/Shutterstock.com
In a recent study published in the Proceedings of the National Academy of Sciences, researchers investigated whether scaffold vaccination can mitigate or prevent infections associated with orthopedic devices.
Why staph infections complicate orthopedic implants
Staphylococcus aureus is the leading global cause of bacterial mortality, responsible for over a million deaths every year. Medical implant devices elevate the risk of S. aureus infection, with orthopedic device infection being particularly devastating due to the need for extended antibiotic treatment and revision surgeries.
Vaccination could be an attractive strategy for individuals requiring device implantation. However, multiple vaccine trials have failed to prevent S. aureus infection after surgery.
The authors previously developed an alternative vaccine platform based on a biodegradable, injectable scaffold of mesoporous silica rods, which contain aligned nanopores for delivering granulocyte-macrophage colony-stimulating factor to recruit dendritic cells (DCs). Scaffold vaccines with pathogen-associated molecular patterns (PAMPs) from Escherichia coli provide mortality benefit upon Enterobacter infection, suggesting PAMPs may induce broad immunity.
PAMP-loaded scaffolds outperform bolus vaccination strategies
In the present study, researchers investigated whether scaffold vaccination can prevent or mitigate staphylococcal infections associated with orthopedic devices. Mice received a subcutaneous injection of saline (naïve), scaffold containing chemokine and adjuvant (scaffold no-antigen), bolus vaccine (containing chemokine, antigen, and adjuvant in saline), or scaffold vaccine (containing chemokine, antigen, and adjuvant) on day 0. PAMPs derived from the S. aureus Xen29 strain were used as the vaccine antigen.
Mice were euthanized on day 7, and their spleens and injection site tissues were harvested. Spleens from the vaccine scaffold group were nearly three- and two-times as heavy as those from the naïve and scaffold no-antigen groups, respectively. There was a trend towards an increase in the number of cluster of differentiation 11c-positive (CD11c+) cells, typically representing DCs, at the injection site in the scaffold vaccine group.
Spleens from the scaffold vaccine group had significantly more CD11c+ cells, a majority of which (>72 %) co-expressed major histocompatibility complex class II (MHC II), a marker of DC activation. Furthermore, the scaffold vaccine group had significantly higher combined levels of serum cytokines associated with the T helper 1 cell (Th1) phenotype, including interleukin (IL)-2, IL-7, IL-1β, IL-12p70, tumor necrosis factor-alpha, and interferon-gamma (IFN-γ), compared to the naïve group.
The bolus vaccine and scaffold vaccine groups had significantly higher Th17-associated cytokines than the naïve group. Next, vaccinated splenocytes were re-exposed to the bacterial antigen to assess cell-mediated immunity. IFN-γ expression was measured as a surrogate for antigen-specific Th1-mediated response. Only mice that received antigen-containing vaccines exhibited significantly elevated expression of IFN-γ compared to naïve mice.
Notably, the scaffold vaccine group showed significantly greater IFN-γ expression compared to the bolus vaccine group. Further, vaccinated animals were challenged with S. aureus orthopedic device infection on day 35. Naïve mice were uninfected following implantation (uninfected) or infected without vaccination (untreated). Other groups were challenged with 1,000 colony-forming units (CFUs) of S. aureus Xen29.
Two weeks later, only the untreated group exhibited persistent weight loss relative to uninfected controls. All infected groups showed higher anti-S. aureus total immunoglobulin G (IgG), with scaffold vaccination resulting in substantially higher anti-S. aureus titers than the scaffold no-antigen, untreated, and uninfected groups. Animals were euthanized on day 49 to harvest implants and collect biofilm-embedded microbes. No bacteria were recovered from the uninfected group.
Bacteria were recovered from other groups, with the scaffold vaccine group having the least bacterial burden. Notably, a subset of scaffold-vaccinated mice exhibited no detectable bacteria on the implant, suggesting potential sterilizing immunity in some cases. In addition, the reduction in bacterial load with scaffold vaccination represented an approximately 2.4-log (roughly 250-fold) decrease relative to untreated controls, indicating a large magnitude of protection.
Scaffold-elicited antibodies recognize multiple staph strains
The team investigated whether scaffold vaccination would protect against different strains of S. aureus. Sera from the scaffold vaccine group were tested against other methicillin-resistant S. aureus (MRSA) strains (JE2 and NRS699lux) and methicillin-susceptible S. aureus strains (UAMS-1 and RN4220). Sera from scaffold vaccine recipients had total IgG with significant binding against all tested strains.
Further, non-vaccinated mice and scaffold vaccine recipients were challenged with implants inoculated with the MRSA strain, NRS699lux, instead of Xen29. Implants of mice that received the scaffold vaccine had a significantly lower burden of NRS699lux at the end of the experiment.
Finally, iron-regulated surface determinant B (IsdB), the second most abundant protein within the PAMP pool used, was evaluated as the vaccine antigen. Mice were vaccinated with bolus IsdB, scaffold IsdB, or the PAMPs-based scaffold vaccine and challenged with Xen29 infection. Scaffold vaccination with either PAMPs or IsdB as the antigen was superior to bolus IsdB in reducing bacterial burden.
Scaffold delivery drives strong implant infection defense
Scaffold vaccination with S. aureus Xen29 PAMPs as the antigen was well tolerated, successfully eliciting Th1-associated immunity and decreasing bacterial burden in mice with orthopedic device infection. Its protective effect was generalizable to another S. aureus strain.
Moreover, scaffold vaccination based on a protein antigen alleviated infection. Overall, scaffold vaccination may facilitate more robust immunity in cases where conventional bolus vaccines have been ineffective.
Download your PDF copy now!
Journal reference:
-
Tatara AM, Lightbown S, Kang S, et al. (2025). Scaffold vaccination for prevention of orthopedic device infection. Proceedings of the National Academy of Sciences, 122(45), e2409562122. DOI: 10.1073/pnas.2409562122. https://www.pnas.org/doi/10.1073/pnas.2409562122