Anesthesiologist and other researchers from Michigan Medicine, Ann Arbor, New York Medical College, Valhalla and Center for Consciousness Science, University of Michigan Medical School, Ann Arbor, have reported a case series of critically ill coronavirus disease 2019 (COVID-19) patients who have developed neuropsychological symptoms after having been discharged from the hospital.
Their study titled, "Delirium and Post-Discharge Neuropsychological Outcomes in Critically Ill Patients with COVID-19: an Institutional Case Series," is now available on the preprint server medRxiv.*
Background
We are in the middle of a pandemic caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) – the causative agent of COVID-19 – as declared by the World Health Organization (WHO) in March 2020. The pandemic has infected over 50 million people worldwide, which has resulted in over 1.25 million deaths. Hundreds of thousands of individuals with the infection have developed critical COVID-19, necessitating hospitalization and even intensive care treatment.
Neurological complications of COVID-19
COVID-19 has been known to cause several neurological symptoms and complications such as encephalopathy (inflammation of the brain), delirium, strokes, seizures, and abnormal movements called ataxia.
One of the most common complications of severe COVID-19 is delirium, explain the researchers. It has been reported in 65 to 80 percent of those patients who needed intensive care unit (ICU) hospitalization. This is usually caused by the virus's attack on the central nervous system and associated inflammatory responses that cause cognitive damage. The risks are raised due to associated factors such as social isolation and sedation during ICU stay.
Questions remain about delirium
Despite such a high incidence of delirium among patients with severe COVID-19, this condition's actual clinical course is not clearly understood. The authors of this study speculate several contributing factors such as the use of multiple medications, associated inflammation, strokes, and vascular events within the brain. They write that these factors need to be clearly understood in their contribution to neurological effects in severe COVID-19.
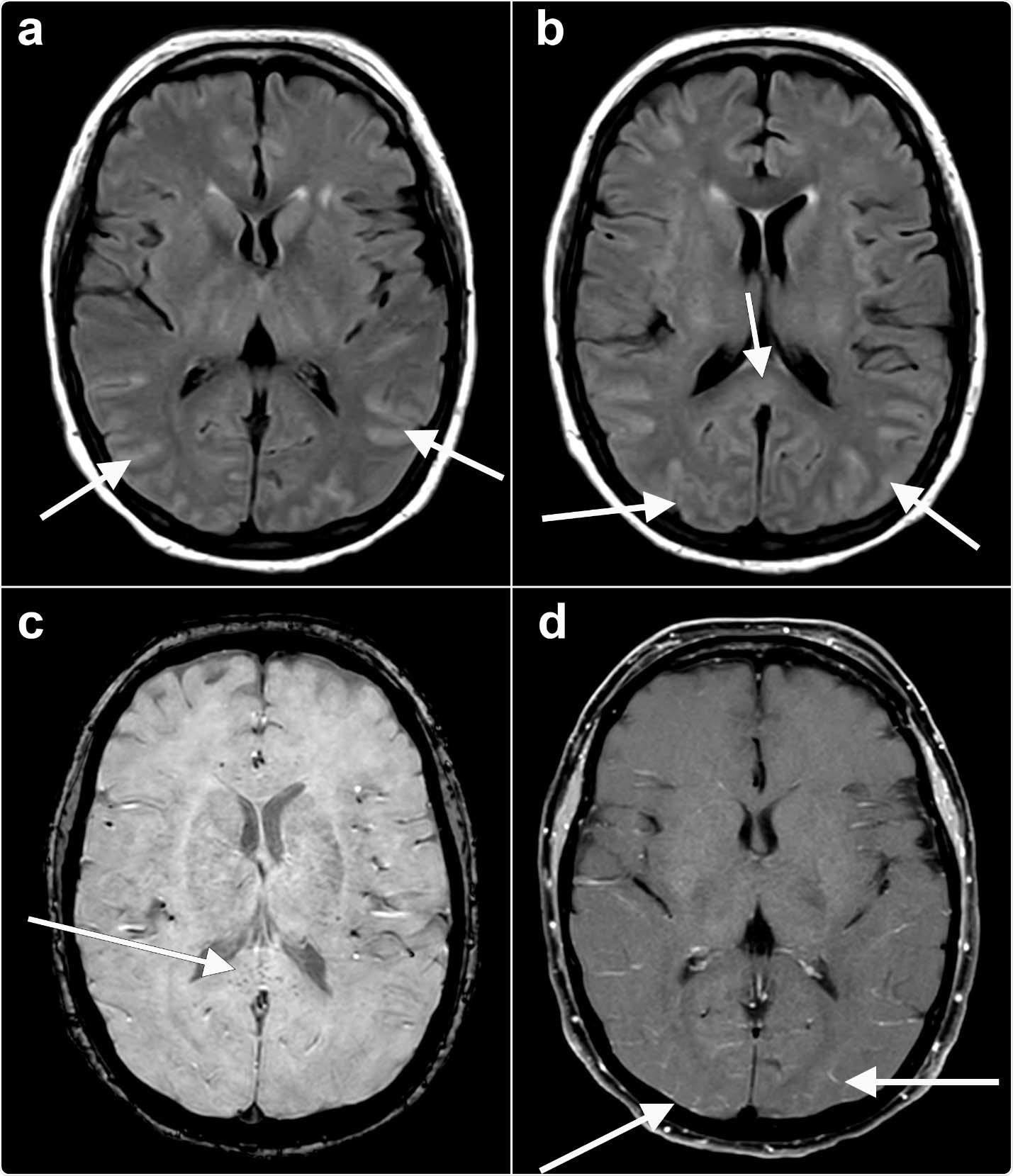
Axial fluid-attenuated inversion recovery (FLAIR) (a, b) images at the level of the basal ganglia show abnormal FLAIR hyperintense signal (arrows) affecting the bilateral occipital, temporal lobes. This appears almost sulcal suggesting a higher protein component within the cerebrospinal fluid. Note the elevated FLAIR signal in the splenium of the corpus callosum (arrow) suggesting parenchymal insult. Axial susceptibility weighted imaging (SWI) (c) at the level of the splenium of the corpus callosum shows small areas of susceptibility (arrow) in the splenium, likely related to microhemorrhage. Axial T1 (d) postcontrast with fat suppression at the level of the basal ganglia shows subtle, though true, enhancement (arrows) in the posterior sulci, arachnoid pial (leptomeningeal) pattern suggesting a degree of encephalitis.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Study design
This was a retrospective chart review of cases at a single center at Michigan Medicine. Chart details were collected from critically ill patients with COVID-19. After their discharge from the hospital, these patients were interviewed via telephonic surveys to detect neurological deficits. The data was collected between 1st March and 31st May 2020.
Some of the main questions asked were:
- Presence of delirium at any point during admission
- Duration of delirium (in days)
- Clinical course of the delirium
- Use of antipsychotic drugs
- Duration of hospital stay
- Duration of ICU stay
- Days requiring ventilator support
- Laboratory values including white blood cell count, C-reactive protein, ferritin, lactate dehydrogenase, d-dimer and interleukin-6.
- New psychiatrist consultation
- New use of antidepressants
- Final outcome after discharge, including stay at home, stay at long term care facilities or death.
- All data on neuroimaging studies
- Telephonic interviews within 30 to 60 days after hospital discharge to check for subjective or objective signs of cognitive impairment. The tests used were, "Patient-Reported Outcomes Measurement Information System (PROMIS) Cognitive Function Abilities 4a, Short Blessed Test (score 0-4 = normal cognition, score 5-9 = questionable impairment, score ≥10 = impairment consistent with dementia),28 Family Confusion Assessment Method for delirium, and the Patient Health Questionnaire-9 (scores ≥10 were considered positive screens for depression)".
Prevention strategies for delirium, including "ABCDEF ICU liberation bundle," were also assessed. Some of the prevention strategies of delirium among the patients were:
- Assess and treat for pain
- Discontinue physical restraints
- Structured mobility exercises
- Removal of temporary medical lines or devices
- Place familiar objects from home at the bedside
- Family education and reassurance
- Promote use of visual and hearing aids
- Sleep promotion protocols (e.g., lights off at night, melatonin tablets)
- Spontaneous awakening trials
Findings
Most of the patients presenting with delirium and neuropsychological impairments after severe COVID-19 were African-American and non-Hispanic. They commonly had comorbidities such as hypertension, Diabetes mellitus, and obesity. Overall results of this study were:
- Delirium incidence was seen among 107 of the total 148 patients (72 percent)
- The median duration of delirium was 10 days (ranging between 4 and 17 days)
- The most common delirium prevention measure was assessment and treatment for pain; the least commonly used measures were providing objects familiar to the patient and using spontaneous awakening trials
- New antidepressant use was seen commonly among those with delirium (24 percent patients or 26 among 107 patients) compared to those without delirium (4 out of 41 or 9.8 percent)
- Psychiatry consultation was needed by 20 percent of those with delirium and 0 percent among those without delirium.
- Improvement in delirium was not seen among any patients during their hospital stay
- Median duration of hospital stay was 25 days and median duration of ICU stay was 15 days
- Length of hospitalization, ICU stay, and need for mechanical ventilation lengthened the duration of delirium in patients
- Sedative-hypnotic drug use was among those with delirium
- These delirium patients had higher markers for inflammation such as WBC, CRP, LDH and d dimer.
- The final disposition of 38 percent of delirium patients was a skilled care facility after discharge.
- 23 percent of patients had cognitive impairment after discharge from the hospital
- 12 percent of patients with delirium tested positive for depression after discharge
Conclusions and implications
The authors of the study suggest the delirium is a serious and common complication seen among those with severe COVID-19. This was likely to be prolonged, especially with a prolonged ICU stay. Authors conclude, "Further research should aim to identify independent risk factors in this population and novel, effective prevention strategies."

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Delirium and Post-Discharge Neuropsychological Outcomes in Critically Ill Patients with COVID-19: an Institutional Case Series Jacqueline Ragheb, Amy McKinney, Mackenzie Zierau, Joseph Brooks, Maria Hill-Caruthers, Mina Iskander, Yusuf Ahmed, Remy Lobo, Phillip E. Vlisides medRxiv 2020.11.03.20225466; doi: https://doi.org/10.1101/2020.11.03.20225466, https://www.medrxiv.org/content/10.1101/2020.11.03.20225466v1
- Peer reviewed and published scientific report.
Ragheb, Jacqueline, Amy McKinney, Mackenzie Zierau, Joseph Brooks, Maria Hill-Caruthers, Mina Iskander, Yusuf Ahmed, Remy Lobo, Graciela Mentz, and Phillip E. Vlisides. 2021. “Delirium and Neuropsychological Outcomes in Critically Ill Patients with COVID-19: A Cohort Study.” BMJ Open 11 (9): e050045. https://doi.org/10.1136/bmjopen-2021-050045. https://bmjopen.bmj.com/content/11/9/e050045.