Human coronaviruses (HCoV) has evolved through environmental changes and adversities that have supported the emergence of novel coronaviruses like the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which is the virus responsible for the current coronavirus disease (COVID-19) pandemic. Aside from COVID-19, currently known HCoVs that can infect humans include α-CoVs such as HCoV-229E and HCoV-NL63, or β-CoVs such as HCoV-HKU1, HCoV-OC43, SARS-CoV, the Middle East respiratory syndrome coronavirus (MERS-CoV), and SARS-CoV-2.
SARS-CoV, MERS-CoV and SARS-CoV-2 are known to produce asymptomatic, mild, or severe respiratory syndromes with fatality rates of 10%, 35%, and 6%, respectively. SARS-CoV and MERS-CoV are zoonotic in nature and are known to infect civet cats and camels, respectively.
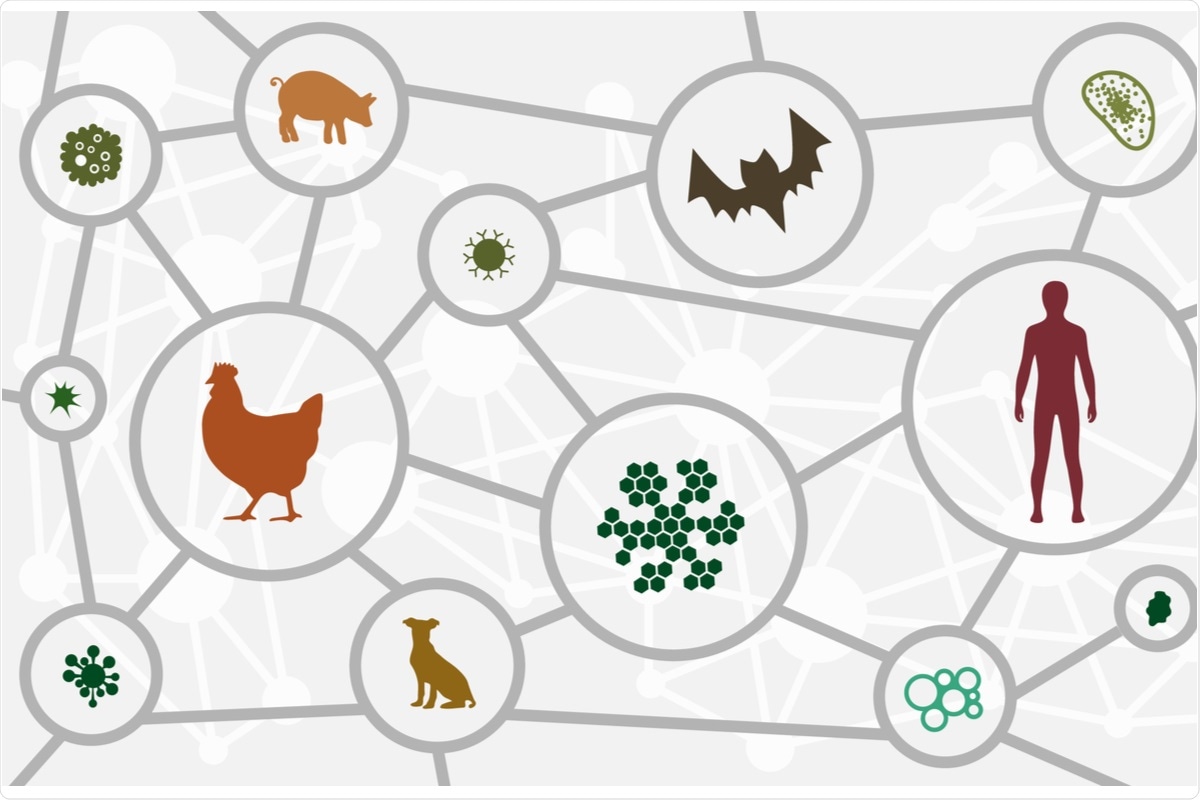 Study: SARS-CoV-2 at the human-animal interphase: A review. Image Credit: magic pictures / Shutterstock.com
Study: SARS-CoV-2 at the human-animal interphase: A review. Image Credit: magic pictures / Shutterstock.com
The first reported case of COVID-19 was found to arise due to the transmission of SARS-CoV-2 from animals to humans in the wet markets of Wuhan, China, in 2019. Since then, SARS-CoV-2 has infected over 264 million worldwide and led to the deaths of over 5.2 million.
In a recent Heliyon review article, researchers summarize the possible causes and routes of transmission of SARS-CoV-2 between humans and animals. Furthermore, the researchers of this article explore the causes of direct interspecies transmission from animals to humans and vice-versa.
Modes of SARS-CoV-2 transmission
SARS-CoV-2 is considered a zoonotic virus with animal(s) serving as its reservoir and intermediate hosts. Few studies have investigated the role of animals as the origin of SARS-CoV-2 infection.
The first of these theories suggest that the virus crossed the species barrier to enter the human population from an animal source at the Wuhan market. Another theory suggests that the virus was first introduced to the market by an infected human who transmitted the virus to an amplifying animal. This animal later spread it to more humans. None of these theories have been proven, even after collecting and testing animal samples from the Wuhan wet market.
Animal reservoirs for coronaviruses were first reported in China in 2019 from virus samples isolated from Malayan pangolins which were found to be 99% genetically identical to the SARS-CoV-2. Another study reported that SARS-CoV-2 bore more similarity to Beta CoV/bat/Yunnan/RaTG13/2013 virus and only 92.4% to the pangolin coronavirus. Despite these discrepancies, these findings highlight a zoonotic origin and a common ancestral background for SARS-CoV-2.
Civet cats are known intermediate hosts for SARS-CoV and camels for MERS-CoV. These findings also give credence to the fact that animals can serve as a reservoir for SARS-CoV-2. Owing to the genetic similarity between SARS-CoV-2 and SARS-CoV, researchers have considered the importance of the intermediate host at the human-animal interface as opposed to focusing solely on the origin of the virus itself.
For the virus to cross the species barrier, there needs to be an infected animal, infectious secretions, and close contact of the animal, possibly repetitively with the sources of infection. Since China has been involved in the consumption and illegal trade of wild animals including Chinese pangolin (Manis pentadactyla) and tiger (Panthera tigris), hunters, traders, and consumers tend to come in either direct or indirect contact with wild animals.
Further, both wild and domestic animals come in contact with each other in market areas. Studies have suggested that more than one billion instances of direct and indirect contacts among wild and domestic animals and humans from the wildlife trade annually.
Bats have been shown as the evolutionary carriers of both alpha and beta coronaviruses, while birds for gamma and delta coronaviruses. Among the four identified lineages of beta coronaviruses, human, murine, porcine, equine, rabbit, camel, bovine, and antelopes have been recognized to support replication of lineage A, whereas humans, bats, and palm civet support replication of lineage B. Thirdly, camels and bats support the replication of lineage C, while bats alone support replication of lineage D.
To date, only eleven animal species are known to become infected with SARS-CoV-2. Naturally-acquired infection of a SARS-CoV-2 susceptible animal requires close contact with COVID-19 infected humans.
Among domesticated animal settings, cats (Felis catus), dogs (Canis lupus familiarise), and ferrets (Mustela putorius furo) were the first reported to have naturally acquired SARS-CoV-2 infection. Cats and ferrets were reported to be highly susceptible to SARS-CoV-2, while dogs only experienced a mild infection.
Among captivated zoo animals, lions (Panthera leo), tigers (Panthera tigris), minks (Neovison vison), snow leopards (Panthera uncia) pumas (Puma concolor), gorillas (Gorilla gorilla), and otters (Lutra canadensis) were also found to be naturally infected by SARS-CoV-2.
Infection induced in laboratory-controlled environment showed that domestic cats (Felis catus), dogs (Canis lupus familiaris), ferrets (Mustela putorius furo), American mink (Neovison vison), Syrian hamsters (Mesocricetus auratus), Egyptian fruit bats (Rousettus aegyptiacus), Roborovski’s dwarf hamster (Phodopus roborovskii), deer mice (Peromyscus maniculatus), bushy-tailed woodrats (Neotoma cinerea), striped skunks (Mephitis mephitis), bank voles (Myodes glareolus), rhesus macaques (Macaca mulatta), cynomolgus macaques (M. fascicularis), African green monkeys (Chlorocebus sp.), Chinese tree shrews (Tupaia belangeri chinensis), common marmosets (Callithrix jacchus), raccoon dogs (Nyctereutes procyonoides), raccoons (Procyon lotor), white-tailed deer (Odocoileus virginianus), laboratory rabbits (Oryctolagus cuniculus), and transgenic mice (Mus musculus) exhibit infection and virus-shedding characteristics.
Moreover, there is an ever-increasing instance of natural exposure of different farm and zoo animals to SARS-CoV-2. However, farm animals that have shown resistance to SARS-CoV-2 infection include cattle (Bos taurus), chicken, ducks, pigs, cottontail rabbits (Sylvilagus sp.), fox squirrels (Sciurus niger), Wyoming ground squirrels (Urocitellus elegans), black-tailed prairie dogs (Cynomys ludovicianus), house mice (Mus musculus), and big brown bats (Eptesicus fuscus).
Contrary to popular belief, the interspecies transmission of SARS-CoV-2 does not necessarily result in clinical disease. Comparatively, most human COVID-19 cases result in subclinical or mild infections.
Cross-contamination from carcasses of wild animals, especially body fluids, as well as digestive, reproductive, and respiratory parts of edible animals, is also being explored as a possibility. However, the exact link between animal and human transmission still remains unsolved.
Implications
More research studies are needed to trace the development of SARS-CoV-2 in animal and human hosts. These studies would also be helpful in studying the effects of mutations in vaccinated individuals and help in formulating improved vaccines.
SARS-CoV-2 continues to mutate and the global medical community rushes to keep up with the emergence of new variants. Finding the exact link between animal and human transmission of SARS-CoV-2 may take more time; however, it is essential that humans continue to abide by physical distancing, masking, and vaccination norms to remain safe in the current COVID-19 pandemic.