Can everyday medications impact your body’s most important systems? A genetic study reveals how common painkillers can reshape your gut’s microbiome.
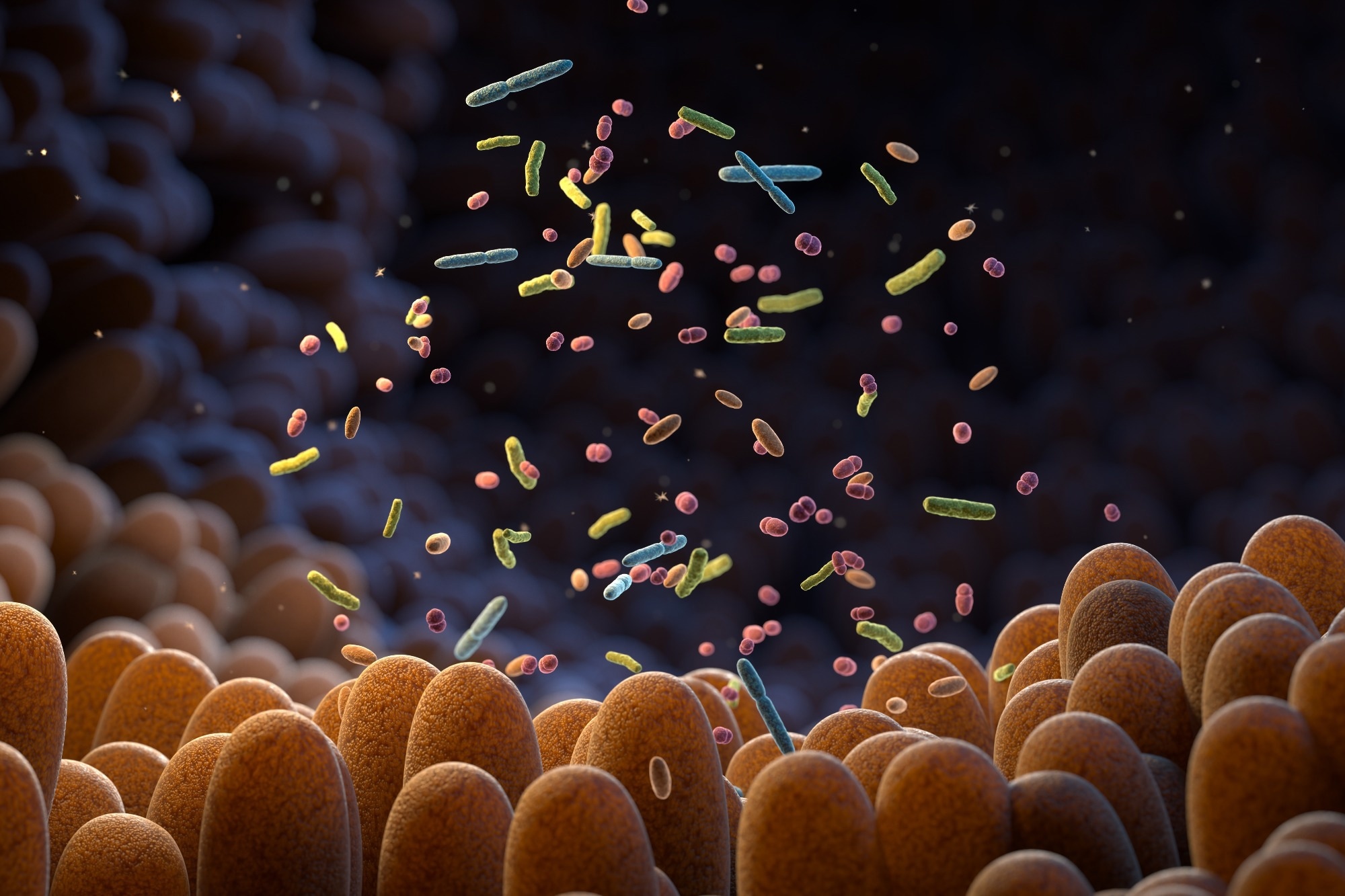 Study: Assessing the impact of common pain medications on gut microbiota composition and metabolites: insights from a Mendelian randomization study. Image credit: Tatiana Shepeleva/Shutterstock.com
Study: Assessing the impact of common pain medications on gut microbiota composition and metabolites: insights from a Mendelian randomization study. Image credit: Tatiana Shepeleva/Shutterstock.com
A study published in the Journal of Medical Microbiology revealed that long-term use of salicylic acid-based painkillers may substantially alter gut microbiota composition and circulating metabolite levels.
Background
The human gut microbiota is crucial in regulating various physiological functions, including metabolic, immune, and neurological functions. The bidirectional communication network between gut microbiota and the brain is referred to as the gut-brain axis, and it has a broad impact on overall health.
The gut-brain axis has gained significant attention in the scientific world due to its involvement in several human diseases, including digestive, immunological, and neuropsychiatric disorders.
Chronic pain is a condition of persistent discomfort that can affect a person's physical and mental health. The condition is primarily treated with analgesics, including opioids, anilides, nonsteroidal anti-inflammatory drugs (NSAIDs), and salicylic acid, which are known to have gastrointestinal side effects.
Emerging evidence suggests that analgesics may affect the functionality of the gut-brain axis, as analgesic receptors are expressed in the gastrointestinal tract and brain. Long-term use of analgesics has been found to alter the composition of gut microbiota and circulating levels of gut microbiota-derived metabolites. However, the causal association between these three factors remains uncertain.
Given the increasing use of analgesics and the significant impact of the gut-brain axis on human health, the current study investigated the causal association between common analgesics and gut microbiota.
The study
The study used the Mendelian randomization approach to determine causal associations between genetic susceptibility to four common analgesics used (NSAIDs, salicylic acid, opioids, and anilides) and changes in gut microbiota composition and circulating metabolites.
The Mendelian randomization approach uses genetic variants as the key variables to infer causal relationships between exposures and outcomes; this study uses analgesics and gut microbiota-related alterations, respectively. This approach can effectively rule out the possible bias caused by confounding factors and reverse causality.
It is important to note that this method assesses genetic predisposition to medication use as a substitute for long-term drug exposure rather than measuring the effects of directly taking these medications in a clinical trial.
Summary-level data on analgesic use and gut microbiota were derived from genome-wide association studies primarily involving European ancestry cohorts, including 466,457 participants from the UK Biobank and 18,340 individuals from the MiBioGen consortium.
Study findings
The study reported a significant impact of salicylic acid use on the abundance of gut microbiota. Specifically, salicylic acid use was associated with a reduced abundance of eight microbiota traits, including genus Clostridiumsensustricto1, Adlercreutzia, Akkermansia, family Clostridiaceae1, and Verrucomicrobiaceae, phylum Verrucomicrobia, class Verrucomicrobiae, and order Verrucomicrobiales and an increased abundance of the family Prevotellaceae.
The study did not find any significant impact of anilide and opioid use on the gut microbiota composition. Conversely, NSAID exhibited only one causal association with the increased abundance of group Eubacterium xylanophilum.
Regarding circulating metabolites, the study found significant causal associations of salicylic acid use with four metabolites, including acetoacetate, creatinine, omega-3 fatty acids, and triglycerides in very large high-density lipoprotein.
Among other tested analgesics, anilide exhibited potential causal associations with three metabolites (citrate, glutamine, and urea), opioid with two metabolites (apolipoproteins and glucose), and NSAID with one metabolite (acetoacetate).
Study significance
The study identifies significant gut microbiota-altering effects of long-term salicylic acid consumption. Notably, the findings suggest that salicylic acid, as a pain relief medication, can exert potential multi-level effects on the gut microbiota composition. However, the study could not find strong associations with gut microbiota regarding other tested analgesics.
Regarding circulating metabolites, the study finds potential causal associations with all four classes of analgesics tested. The metabolites affected by salicylic acid use play crucial roles in brain glucose uptake, memory decay, and Alzheimer’s disease development. Similarly, metabolites affected by anilides and opioids are associated with the pathogenesis of Parkinson’s disease, acute colitis, and schizophrenia.
However, these links are not the direct effects observed in this study; they are discussed as possibilities based on the known roles of these metabolites in disease.
Overall, the study findings highlight the need for future investigations to more conclusively understand the extent to which analgesics can potentially trigger the pathogenesis of neuropsychiatric and digestive disorders through the gut-brain axis.
This study is the first of its kind to apply Mendelian randomization to assess the causal relationship between analgesic drugs and gut microbiota. Multiple methods were used to accurately generate Mendelian randomization estimates and substantially improve the robustness of observed associations.
Despite robust methodologies, the study has some limitations. Many factors, including diet, physical activity, and other lifestyle habits, can influence gut microbiota composition. The study analysis did not control for these confounding factors. Further investigations are needed to uncover the underlying mechanisms.
Furthermore, the Mendelian randomization analyses were conducted based on the assumption of linear correlation, limiting the possibility of ruling out a nonlinear relationship between exposure and outcome.
While these results provide evidence of potential causal relationships between certain analgesics and changes in gut microbiota and metabolites, direct clinical studies are needed to confirm these effects and clarify their clinical significance.
Download your PDF copy now!