The 23-year ERSPC trial reveals that sustained, protocolized PSA testing lowers prostate cancer deaths and improves the benefit-to-harm ratio, supporting a shift toward risk-based, patient-centered screening strategies.
European Study of Prostate Cancer Screening - 23-Year Follow-up. Image Credit: Joseph Kelly / Shutterstock
In a recent study published in The New England Journal of Medicine, investigators reported the final 23-year analysis of the European Randomized Study of Screening for Prostate Cancer (ERSPC), quantifying benefits, harms, and practice implications.
Balancing Early Detection and Screening Harms
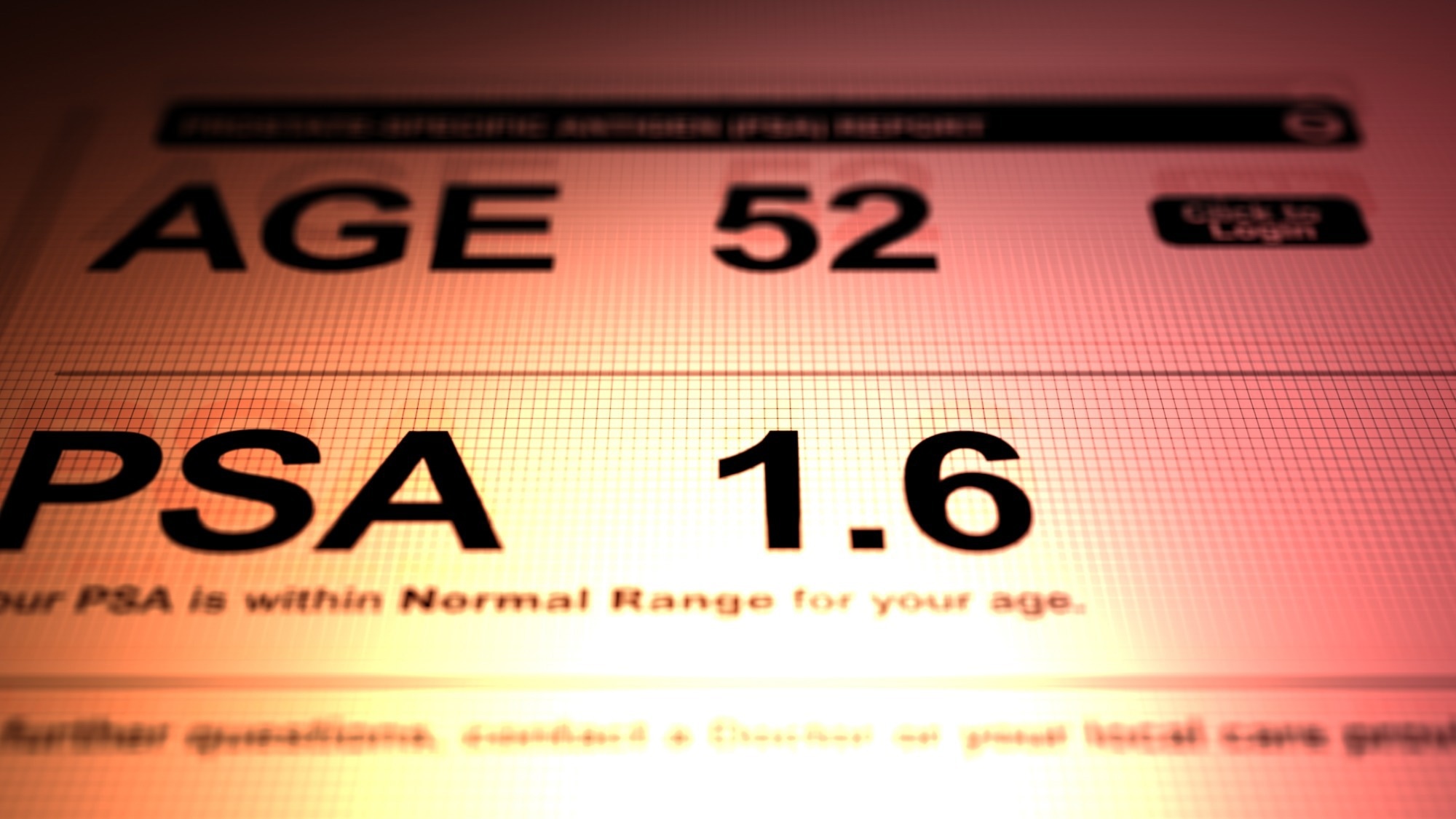
Prostate-related evaluation is common in aging men, and screening policies must balance earlier detection with potential harms. Prostate-specific antigen (PSA) offers earlier detection; however, its promise must be balanced against the risks of false positives, biopsies, and treatment side effects. Overdiagnosis of indolent tumors can provoke anxiety and procedures that may not extend survival. Meanwhile, longer lifespans mean more years at risk, and prostate cancer deaths are projected to rise globally. Health systems need evidence to weigh the reduction in mortality against the quality of life and available resources. Further research should refine risk-based screening to preserve benefits while minimizing unnecessary tests and treatments.
Design of the ERSPC Randomized Screening Trial
Investigators conducted a multicenter, randomized study across eight European countries, focusing on a prespecified core cohort of men aged 55–69 years at the time of randomization. Participants were allocated to either repeated PSA testing with defined biopsy triggers or to a control group that was not invited to screening. Screening was conducted using standardized Hybritech assays; most centers invited men every four years, while Sweden and France invited men every two years, and Belgium invited men every seven years. Common biopsy thresholds were 3.0 ng/mL, with country-specific ancillary testing, such as digital rectal examination or the free-to-total PSA ratio, when results were borderline.
Primary and Secondary Outcomes in the ERSPC
The primary outcome was prostate cancer mortality, adjudicated by blinded local committees using a uniform algorithm, with an international committee resolving disagreements. Secondary outcomes included the incidence overall and by European Association of Urology (EAU) risk categories, as well as advanced disease defined by lymph-node or bone metastases or a PSA level greater than 100 ng/mL.
Statistical Methods and Sensitivity Analyses
Analyses followed intention-to-screen principles. Poisson regression estimated rate ratios (not risk ratios); competing-risk methods accounted for deaths from other causes. Absolute risk differences, the number needed to invite, and the number needed to diagnose were computed with bootstrap resampling. Prespecified and sensitivity analyses explored center heterogeneity and non-attendance effects. Tumor-node-metastasis staging, Gleason scoring, and PSA levels documented clinical severity. French centers were excluded from the primary analysis because participation was below 50% and biopsy compliance was low.
Mortality Reduction and Screening Efficacy at 23 Years
After a median of 23 years, prostate cancer mortality was 1.4% in the screening group versus 1.6% in the control group, corresponding to a 13% relative reduction (rate ratio, 0.87; 95% confidence interval [CI], 0.80–0.95) and an absolute risk reduction of 0.22%. Translated for practice, inviting 456 men to screening prevented one death from prostate cancer, and diagnosing 12 prevented one death. Other-cause mortality was identical at approximately 49% in both groups, indicating that life expectancy conditions the net benefit.
Screening Shifts Cancer Detection Toward Early-Stage Disease
Prostate cancer incidence was higher with screening (rate ratio, 1.30), reflecting the detection of additional low-risk tumors. The rate ratios for low-risk, intermediate-risk, high-risk, and advanced disease were 2.14, 1.10, 0.95, and 0.66, respectively, suggesting a shift toward finding cancers earlier and reducing late presentations.
Screening Compliance and Diagnostic Yield
Compliance was high, as 83% of invited men attended at least one round, 28% had at least one positive PSA test, and 89% underwent biopsy after a positive result. However, only about one in four biopsies (approximately 24%) confirmed cancer. These figures explain why screening increases procedures and diagnoses that may not alter individual outcomes. Analyses adjusted for non-attendance showed a slightly larger benefit (rate ratio, 0.84; 95% CI, 0.76–0.92), consistent with dilution in the primary intention-to-treat estimates.
Consistency Across Centers and Sensitivity Findings
Including French centers with shorter follow-up (median, 17 years) yielded similar results (rate ratio, 0.84; 95% CI, 0.76–0.93). Center-specific differences in screening interval and biopsy compliance contributed to observed heterogeneity.
Durability of Mortality Benefit Over Time
Among men who reached the protocol’s upper age limit without a cancer diagnosis (median 72 years), the mortality advantage persisted long after screening ceased but waned over time; by roughly six years, the upper bound of the 95% CI for the hazard ratio crossed one, indicating diminishing returns in older men with substantial competing mortality.
Comparison with U.S. and U.K. Screening Trials
Placed alongside other landmark trials, these results clarify why design and implementation matter. In the United States PLCO trial, heavy contamination of the control arm by opportunistic PSA testing obscured differences between groups, and modeling suggested that with lower contamination, PLCO results would have been consistent with a 27–32% mortality reduction.
In the United Kingdom CAP trial, a single invitation achieved modest participation (approximately 40%) and resulted in only a small absolute reduction in deaths (an 8% relative and 0.09% absolute reduction at 15 years). Together, these comparisons highlight that repeated, protocolized testing with engagement is necessary to convert early detection into fewer deaths while avoiding excess harms.
Improving the Harm, Benefit Ratio Over Time
At 23 years, the absolute mortality reduction increased from 0.16% at 16 years to 0.22%, while the excess incidence decreased from 31 to 27 per 1,000 men, indicating that the harm-benefit ratio improved over time.
Implications for Risk-Based and Individualized Screening
Long-term, protocolized PSA screening reduces deaths from prostate cancer but increases testing, biopsies, and diagnoses, many for low-risk disease. Shared decision-making should incorporate individual risk, baseline PSA levels, life expectancy, and personal values. Risk calculators and magnetic resonance imaging (MRI) pathways can help decouple an elevated PSA from the need for immediate biopsy, while active surveillance can spare treatment for low-risk tumors.
Recommendations for Optimizing Prostate Screening Policy
Programs should adopt risk-based intervals and consider stopping rules for men with very low midlife PSA or limited longevity. The study noted that very low baseline or age-60 PSA strongly predicts lifetime risk, supporting longer intervals or screening cessation in low-risk men. Overall, targeted screening can preserve mortality benefits, lessen overdiagnosis and overtreatment, and better align care with what matters to patients.
Journal reference:
- Roobol, M. J., de Vos, I. I., Månsson, M., Godtman, R. A., Talala, K. M., den Hond, E., Nelen, V., Villers, A., Poinas, G., Kwiatkowski, M., Wyler, S., Recker, F., Puliti, D., Gorini, G., Zappa, M., Paez, A., Lujan, M., Bangma, C. H., Tammela, T., Schröder, F. H., Remmers, S., Hugosson, J., Auvinen, A., & the ERSPC Investigators. (2025). European Study of Prostate Cancer Screening, 23-Year Follow-up. N Engl J Med. 393(17), 1669–1680. DOI: 10.1056/NEJMoa2503223, https://www.nejm.org/doi/full/10.1056/NEJMoa2503223