Both maternal and infant wellbeing has been substantially impacted due to the coronavirus disease 2019 (COVID-19) pandemic. Infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) during pregnancy has been linked to an increased risk of preterm birth. In contrast, a reduction in preterm births has been reported during community lockdowns in non-infected mothers. However, studies assessing the impact this has on neonatal outcomes are lacking, and the previous studies that consider this issue are from countries with relatively high COVID-19 community transmission rates.
Melbourne, Australia, was subjected to one of the world’s strictest community transmission mitigation measures for a lockdown period of two weeks in 2020. The strict lockdown measures relative to low rates of community transmission provide a unique setting to examine the effects of the lockdown.
It has been suggested that a lack of exposure to infectious pathogens is directly correlated to a reduction in preterm births during lockdown. A team of researchers from Australian institutes examined the consequences of community-wide lockdowns on neonatal outcomes of preterm infants, with a secondary focus on the underlying rates of systemic inflammation in infants and mothers around the time of birth.
A preprint version of this study, which is yet to undergo peer review, is available on the medRxiv* preprint server.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
What was the research methodology?
The authors conducted a retrospective cohort study at Monash Health, Melbourne’s largest public health service, facilitating >1000 births per year. Preterm infants (>20 weeks and <37 weeks gestation) born from mothers with conception dates between 1 November 2019 and 29 February 2020, who would have been between 3 and 19 weeks pregnant when lockdown commenced (exposed group), were compared to preterm infants conceived within the same time period a year before (control group).
The authors focus on a composite of death or significant morbidity for this study, which included chronic lung disease (CLD), necrotizing enterocolitis (NEC), severe intraventricular hemorrhage (IVH), retinopathy of prematurity (ROP), or culture-positive sepsis. The secondary outcomes studied by the authors were the rates of individual preterm complications and differences in inflammatory markers between cohorts.
What did the authors find?
In the exposed group, there was 295/3187 (9.3%) live neonates born <37 weeks, compared to the control group, which had 347/3229 (10.7%) live neonates. The median gestational age for the exposed group was 35+4 weeks versus 35+0 weeks in the control group. In the exposed group, the primary outcome occurred in 36 (12.2%) of infants <37 weeks, compared to 46 (13.3%) infants <37 weeks in the control group.
When the unit of analysis was considered as the mother, the primary outcome due to prematurity occurred in 36/3187 (1.1%) in the exposed group and 46/3229 (1.4%) in the control group of live neonates born before 37 weeks. The secondary outcomes displayed a significant reduction in jaundice, continuous positive airway pressure (CPAP) requirement, hypoglycemia, admission to neonatal intensive care unit >48 hours, and median neonatal intensive care unit length of stay in the exposed group (Table 1).
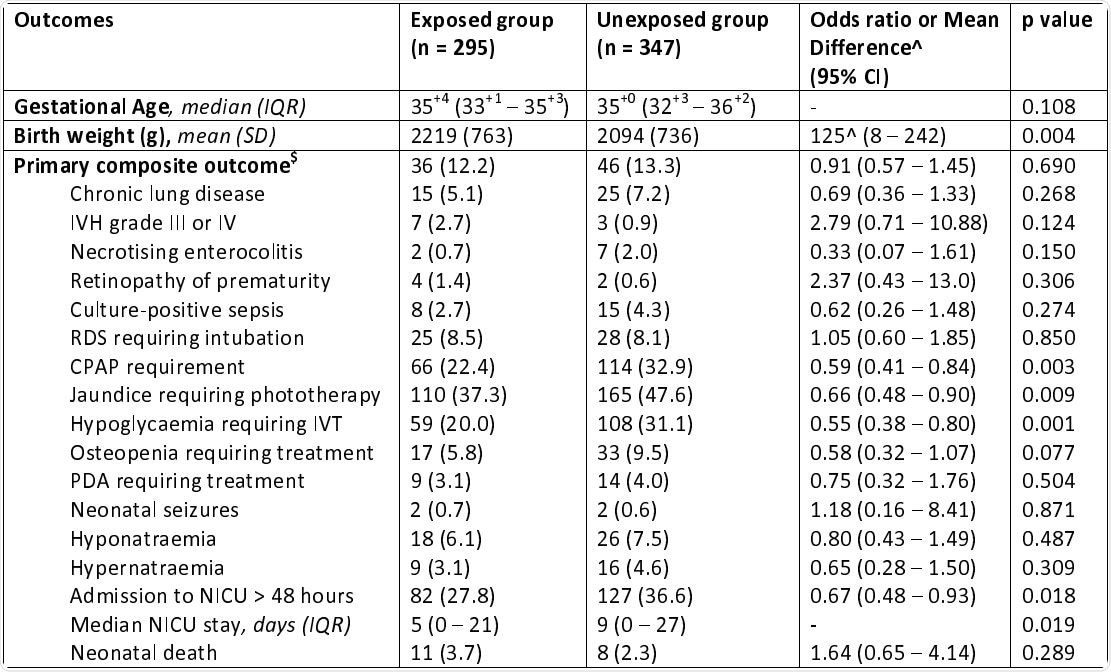
Comparison of neonatal outcomes (live neonates < 37 weeks gestation)
Implications
Although the authors reported a 15% reduction in preterm births <37 weeks gestation within the lockdown group, their findings displayed no significant difference in the composite primary neonatal outcome among preterm infants. Among the preterm infants in the exposed group, there was a 34% reduction in neonatal jaundice, a 41% reduction in CPAP requirement, a 33% reduction in the need for neonatal intensive care unit, and a 45% reduction in hypoglycemia. These reductions in common complications observed in infants could reflect the significantly higher birth weight seen in the exposed group when compared to the unexposed group.
When compared to infants born to mothers who were acutely affected by COVID-19, the results from this study are almost the exact opposite. Infants from mothers affected by COVID-19 displayed increased neonatal intensive care unit visits, jaundice, and respiratory distress. This highlights that the results from this study could be due to the impact of community lockdown alone without high COVID-19 infection rates.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Preterm outcomes following COVID-19 lockdowns, Melbourne, Australia, Brendan Mulcahy, Daniel L. Rolnik, Alexia Matheson, Yizhen Liu, Kirsten R. Palmer, Ben W. Mol, Atul Malhotra, medRxiv, 2021.09.29 https://doi.org/10.1101/2021.09.29.21264295, https://www.medrxiv.org/content/10.1101/2021.09.29.21264295v2
- Peer reviewed and published scientific report.
Mulcahy, Brendan, Daniel L. Rolnik, Alexia Matheson, Yizhen Liu, Kirsten R. Palmer, Ben W. Mol, and Atul Malhotra. 2021. “Preterm Infant Outcomes Following COVID-19 Lockdowns in Melbourne, Australia.” Children 8 (12): 1169. https://doi.org/10.3390/children8121169. https://www.mdpi.com/2227-9067/8/12/1169.