Despite near-perfect exam scores, large language models falter when real people rely on them for medical advice, exposing a critical gap between AI knowledge and safe patient decision-making.
Study: Reliability of LLMs as medical assistants for the general public: a randomized preregistered study. Image Credit: Teacher Photo / Shutterstock
In a recent study published in the journal Nature Medicine, researchers investigated whether large language models (LLMs) can effectively support the general public in navigating common health scenarios.
Although LLMs performed very well when evaluated on their own, participants who used LLMs did not perform better than those using traditional resources and often performed worse. This highlights significant failures in human-LLM interaction that are not captured by standard benchmarks or simulations, and suggests that strong standalone medical knowledge does not necessarily translate into effective real-world user support or improved clinical decision-making by lay users.
Growing Expectations for AI in Patient Health Guidance
Recent advances in artificial intelligence (AI), particularly LLMs, have raised expectations that healthcare access could be expanded by bringing medical knowledge directly to patients. LLMs already achieve near-passing or passing scores on medical licensing exams and are increasingly used by the public for health-related questions, even though benchmark performance may not reflect practical clinical usefulness or real-world patient comprehension.
Surveys suggest that a substantial proportion of adults regularly consult AI chatbots for medical advice, often seeking guidance on sensitive or personal concerns. While these tools show promise, prior research indicates that strong performance on medical standards does not necessarily translate into improved outcomes in real-world clinical settings or into improved decision-making when non-expert users must interpret the outputs, which may sometimes introduce misunderstanding or misplaced confidence.
Studies involving clinicians have shown that AI assistance can fail to improve, or even worsen, diagnostic accuracy when humans must interpret and apply AI output. As a result, some have proposed deploying LLMs directly to patients as an initial interface with the healthcare system. However, whether non-expert users can effectively interpret and act on LLM-generated medical advice remains unclear.
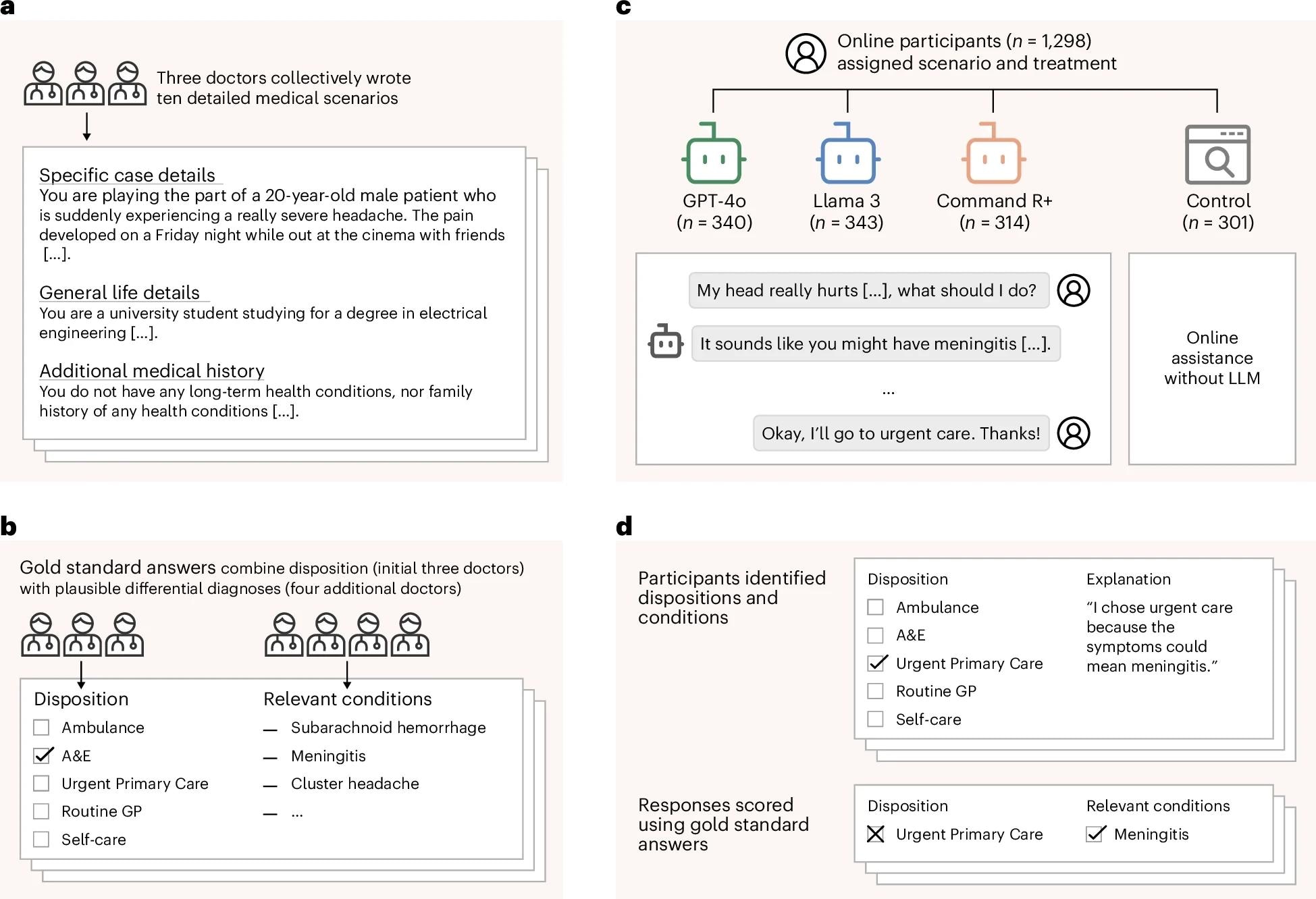
a, Three doctors drafted ten medical scenarios, iteratively revising them until they reached unanimous agreement about the best disposition on a five-point scale from self-care to ambulance. b, Four additional doctors read the scenarios and provided differential diagnoses, which were combined to form gold-standard lists of relevant conditions. c, We recruited 1,298 participants and randomly assigned them to one of four experimental conditions. Each participant was randomly allocated one of ten medical scenarios. The treatment groups conversed with an LLM to help assess the scenarios. The control group was permitted to use any method, with most participants using internet search or their own knowledge. d, Top: participants then chose a disposition and identified medical conditions that motivated their choice. Participants completed two scenarios, until a total of 600 examples were collected for each experimental condition. Bottom: we evaluated each participant’s responses using the gold-standard answers.
Randomized Study Design and Experimental Conditions
Researchers systematically evaluated how members of the general public interact with LLMs when making medical decisions and assessed whether these interactions improve understanding and decision-making compared with conventional approaches.
They conducted a randomized controlled study involving 1,298 adult participants living in the United Kingdom. Participants were presented with realistic medical scenarios designed by physicians, each requiring the user to identify possible underlying medical conditions and select an appropriate disposition or course of action on a five-point scale, with options ranging from calling an ambulance (the most serious response) to self-care (the least serious response).
Three doctors developed and validated the scenarios and agreed on the correct disposition, while four additional doctors generated gold standard lists of relevant diagnoses. Each participant was randomly allocated to one of four groups. Three treatment groups each used a different LLM, GPT 4o, Llama 3, or Command R plus, and a control group could use any resources they normally would, such as internet searches.
Demographic stratification ensured that each group resembled the national adult population. Each participant completed up to two scenarios, resulting in 600 responses per experimental condition. Performance was evaluated by comparing participants’ selected dispositions with physician-agreed answers and by assessing whether listed conditions matched the gold-standard diagnostic lists.
To contextualize the findings, the researchers also evaluated LLMs operating alone on the same scenarios, tested performance on medical knowledge benchmarks, and conducted simulated user experiments in which LLMs replaced human participants.
Human and LLM Interaction Reveals Performance Gaps
When evaluated independently, all three LLMs performed strongly. Each successfully identified one or more relevant conditions in over 90 percent of cases, although correct disposition recommendations were more moderate, averaging roughly half of cases rather than approaching expert-level clinical reliability.
However, when paired with human users, performance declined substantially. Participants using LLMs identified relevant medical conditions in fewer than 35 percent of cases, significantly worse than the control group, which relied on traditional resources such as search engines and established health websites.
Disposition accuracy did not differ significantly between LLM-assisted participants and controls, with both groups frequently underestimating the seriousness of conditions. Analyses of interaction transcripts revealed multiple points of failure. Users often provided incomplete or poorly structured information; LLMs sometimes misinterpreted inputs or generated misleading suggestions; and participants frequently failed to adopt correct recommendations, even when they were presented during the conversation.
Benchmark evaluations using medical licensing style questions showed that high LLM scores did not predict success in interactive settings. Similarly, simulations using LLM-generated patients overestimated real-world performance and failed to capture human variability, with simulated users generally performing better than real participants. Overall, the results demonstrate a consistent gap between LLMs' medical knowledge and their effectiveness when used interactively by non-expert users.
Implications for Safe Deployment and Future Research
This study demonstrates that current LLMs tested in this research setting are not ready for safe deployment as public-facing medical advisors, despite strong standalone performance on medical tasks. A key strength of the work is its focus on real human-LLM interactions, which reveal failures that are invisible to traditional benchmarks and simulations.
The findings suggest that the main challenge lies not only in medical knowledge but also in communication, consistency, and user interpretation. Users struggled to know what information to provide, how to evaluate multiple suggestions, and when to trust or act on LLM output, even when correct information appeared during the interaction. This highlights limitations in both AI communication design and human interpretation skills.
Limitations include the use of hypothetical scenarios rather than real clinical encounters and a focus on common conditions, which may underestimate the challenges posed by more complex cases. Additionally, newer or specialized models may perform differently, and future improvements in conversational design or clinical fine-tuning could alter performance, although whether such gains translate into real-world benefit remains uncertain.
Nonetheless, the study provides a critical lower bound on real-world performance and highlights the risks of premature deployment. The authors concluded that systematic testing with diverse human users should be a foundational requirement before LLMs are used in healthcare. Medical expertise alone is insufficient to ensure safe and effective patient support, and real user evaluation should complement traditional benchmark testing before clinical integration.
Journal reference:
- Bean, A.M., Payne, R.E., Parsons, G., Kirk, H.R., Ciro, J., Mosquera-Gómez, R., Hincapié M, S., Ekanayaka, A.S., Tarassenko, L., Rocher, L., Mahdi, A. (2026). Reliability of LLMs as medical assistants for the general public: a randomized preregistered study. Nature Medicine. DOI: 10.1038/s41591-025-04074-y, https://www.nature.com/articles/s41591-025-04074-y