New research reveals that even low levels of air pollution can trigger dangerous changes in blood vessels, underscoring the urgent need for clean air to protect heart health worldwide.
Review: Air pollution and atherosclerosis
In a recent review article published in the journal Atherosclerosis, researchers provided an overview of how air pollution contributes to the start and worsening of atherosclerosis. They summarized studies linking air pollution exposure to physical changes in blood vessels and explained the biological processes involved. The article synthesizes an important body of literature that highlights the role of air pollution, particularly fine particulate matter (PM2.5), in accelerating atherosclerosis. This condition poses a major cardiovascular health risk and demands urgent global efforts for mitigation.
Background
Cardiovascular disease (CVD) remains the world’s biggest killer, causing over 20 million deaths globally each year. Although global rates of CVD are decreasing, the actual numbers of cardiovascular deaths are still rising in many countries due to aging and expanding populations.
Atherosclerosis, characterized by the buildup of fats (lipids) within the inner lining of arteries, along with inflammatory cells, forming complex, fatty plaques over time, can cause plaque instability, leading to erosion or rupture. This can trigger strokes or heart attacks and is a key contributor to many CVDs.
While traditional risk factors like smoking, high blood pressure, diets high in saturated fat, and low physical activity are well known, environmental factors such as air pollution are now recognized as significant contributors to cardiovascular risk.
Outdoor, or “ambient”, air pollution includes harmful gases like nitrogen dioxide (NO2), sulphur dioxide (SO2), carbon monoxide (CO), and ozone (O3), along with particulate matter (PM) of various sizes (PM10, PM2.5, and ultrafine particles or UFPs/nanoparticles). Ultrafine particles from combustion sources, such as vehicle exhaust (which contain a mix of carbon, organic compounds, and metals), are especially harmful because they can trigger oxidative stress (a type of cell damage) and inflammation, worsening cardiovascular health.
Air pollution was recently ranked (based on data from 2021) as the second greatest risk factor for mortality, and the number one risk factor for what's known as disability-adjusted life years. This equates to between 7-9 million premature deaths globally every year, with approximately 70% linked to cardiovascular events like heart disease and stroke.
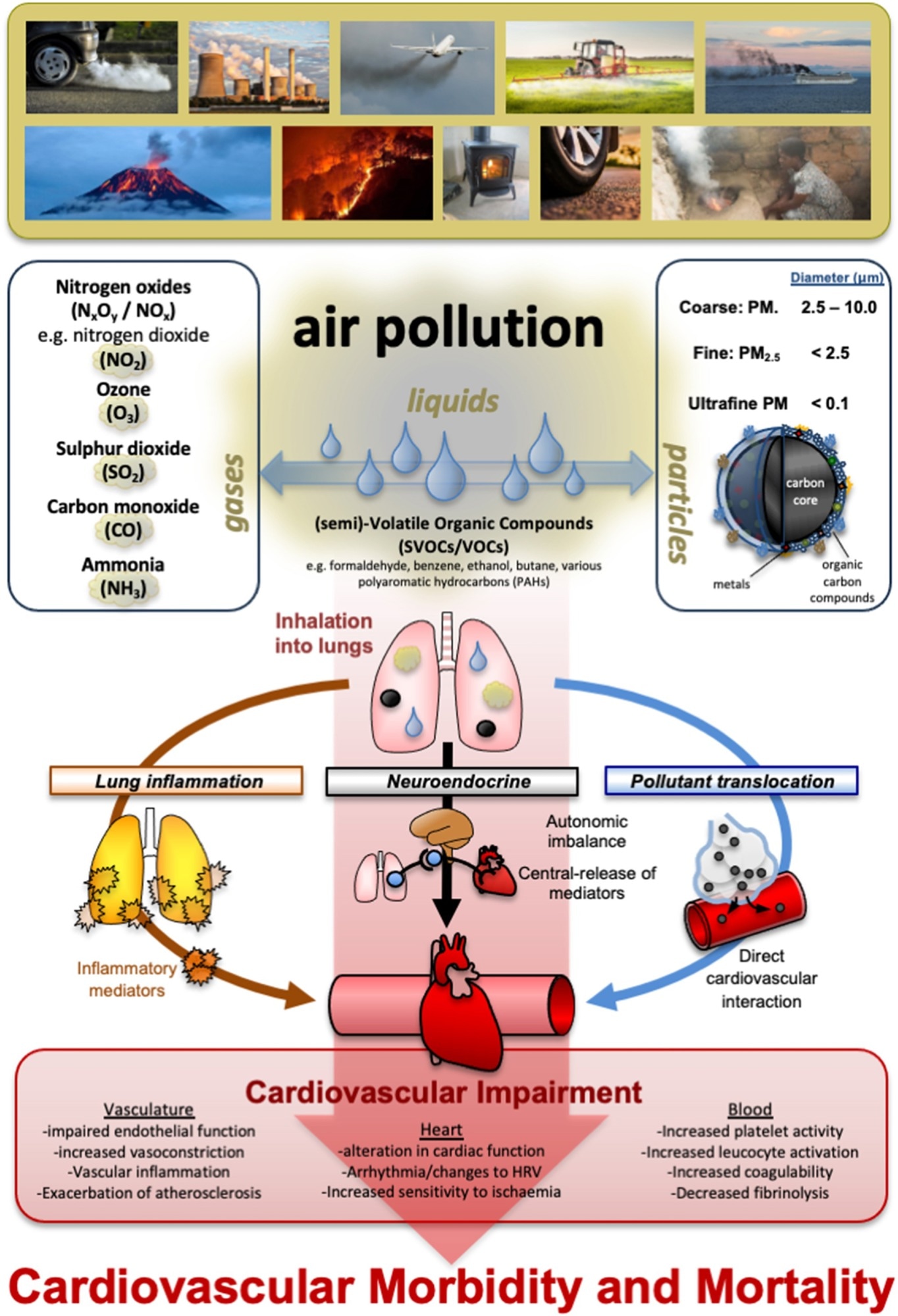
Composition and categorization of air pollution and particulate matter. Top half: Air pollution can arise from many sources and be broadly characterized into gases, particles, and volatile liquids, with particulate matter encompassing particles of different sizes and composition. Lower half: overview of mechanisms linking the inhalation of air pollution to impair cardiovascular function, promote morbidity, and mortality.
Linking air pollution with atherosclerosis
Air pollution is strongly linked to a wide range of cardiovascular diseases, including various forms of heart disease, stroke, hypertension, and other blood vessel problems. Among various pollutants, fine particulate matter (PM2.5) poses the most consistent and greatest risk, though ultrafine PM also poses a significant concern.
Epidemiological studies show that air pollution, especially PM2.5, is associated with early signs and measurable indicators of atherosclerosis, such as increased carotid intima-media thickness (CIMT – a measure of artery wall thickness), coronary artery calcification (CAC – calcium buildup in heart arteries), calcium in the aorta (the body's main artery), and arterial stiffness.
Meta-analyses reveal significant increases in CIMT linked to long-term PM2.5 exposure, though the estimated effect sizes vary, and sometimes the findings are not statistically clear-cut (with confidence intervals just overlapping zero). Evidence is less consistent for PM10 and proximity to traffic, and still relatively limited for gaseous pollutants like nitrogen dioxide (NO2) and ozone (O3), where associations have been more mixed. Black carbon (a marker of soot from burning fuels) and similar carbon-rich particles appear especially harmful.
Recent studies also show that early-life exposure to air pollution, including during pregnancy in some cases, may contribute to adverse vascular changes in children and adolescents. Although findings vary and are not always statistically significant, positive trends point toward long-term cardiovascular risks. PM2.5 exposure has also been associated with the development of "high-risk" plaques (more prone to rupture) in adults.
Despite gaps in evidence, particularly regarding long-term exposure to non-particulate pollutants, the impact of short-term PM exposure on accelerating atherosclerosis, and data from low- to middle-income countries, the overall literature supports a strong association between air pollution and the development and progression of atherosclerosis.
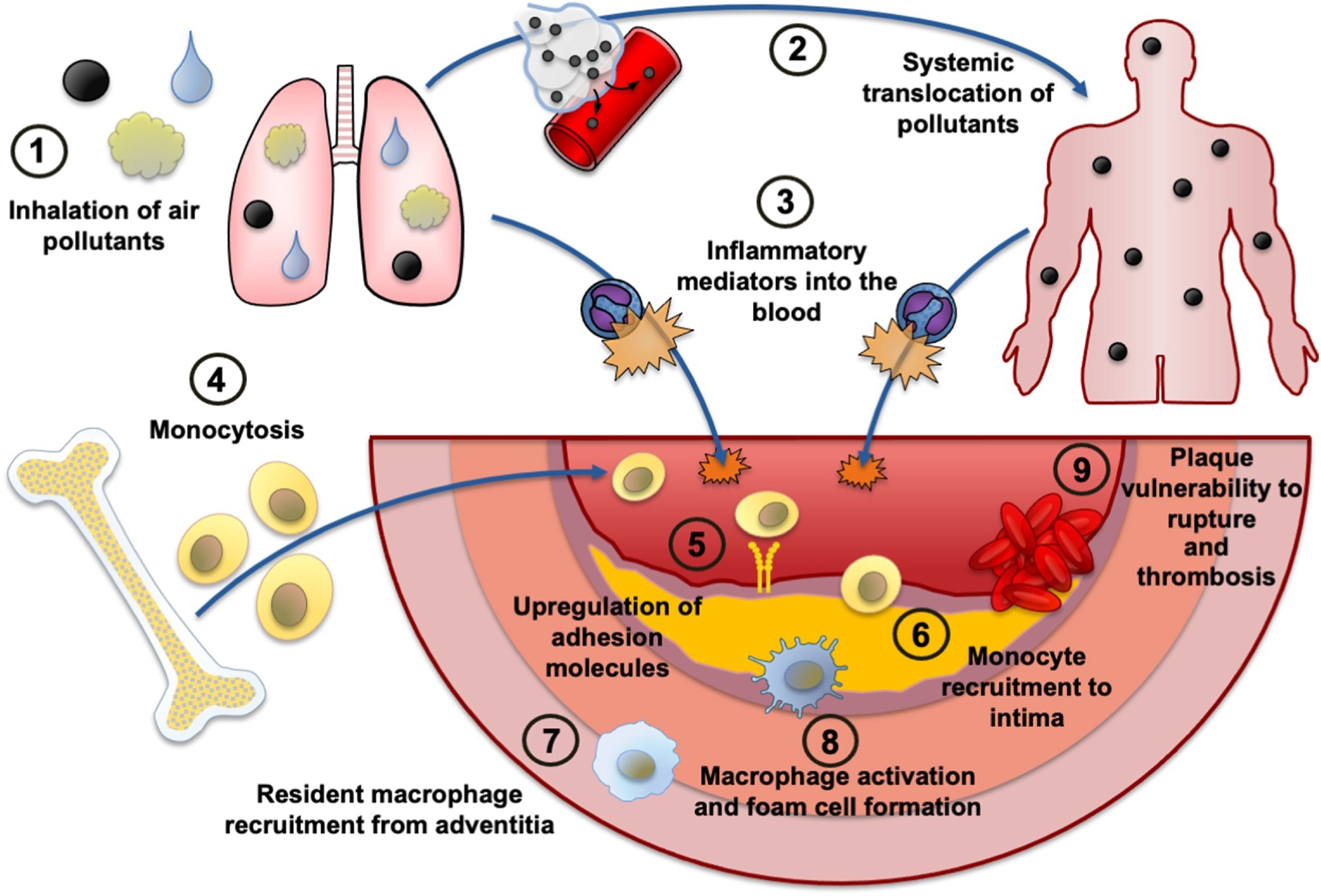 Potential mechanisms by which air pollutants promote atherosclerosis through inflammation.
Potential mechanisms by which air pollutants promote atherosclerosis through inflammation.
Revealing biological mechanisms
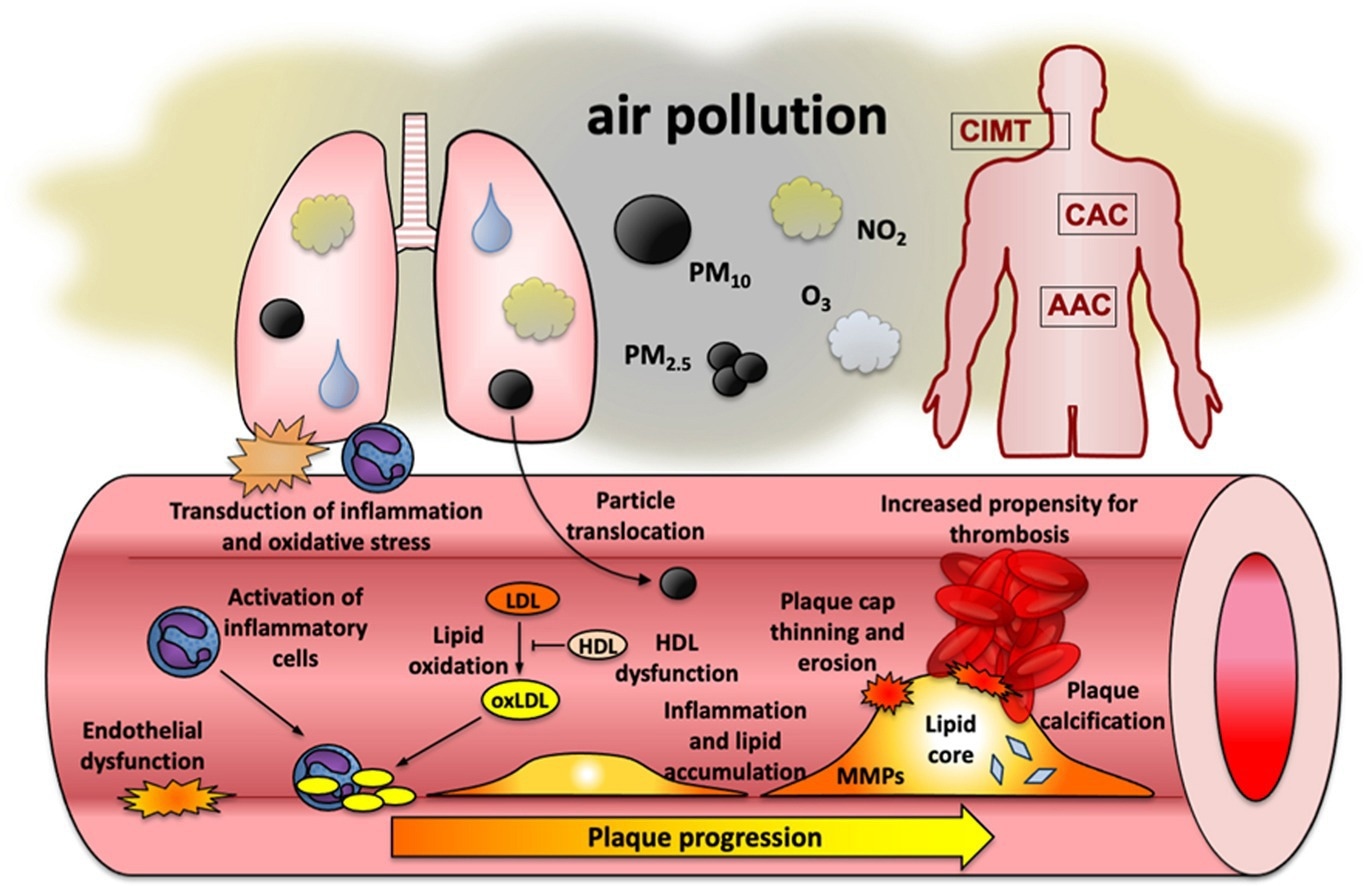
Air pollution, especially fine particulate matter (PM2.5), promotes atherosclerosis through multiple biological pathways.
PM2.5 exposure can lead to harmful changes in blood fats, including increasing "bad" cholesterol (LDL) and impairing the function of "good" cholesterol (HDL), making it less effective at clearing fats from arteries.
It also induces oxidative stress by generating damaging molecules (like reactive oxygen species or ROS). This cellular stress promotes the modification of LDL cholesterol, making it more likely to build up in artery walls and contribute to "foam cell" formation (an early stage of plaque development). Certain gaseous pollutants can also cause this type of stress.
Air pollution triggers systemic inflammation throughout the body. This can happen when pollutants stimulate immune cells in the lungs, which then release inflammatory signals into the bloodstream, or when tiny particles directly activate immune cells. This leads to higher levels of pro-inflammatory substances (like TNF-α and certain interleukins) and encourages more immune cells (monocytes) to travel to and enter developing plaques.
PM exposure damages the lining of blood vessels (endothelial dysfunction), making them "stickier" and allowing more white blood cells to enter the artery wall. Diesel exhaust particles and ozone can worsen this damage, even without the particle component, highlighting the role of harmful gases.
Pollutants also impair the function of macrophages (a type of immune cell), leading to more fat accumulation within them and promoting the death of these cells within plaques. This is partly because the pollutants hinder the macrophages' ability to clear out dead cells (a process called efferocytosis). Other immune cells, like T cells, also contribute to ongoing inflammation in the vessel wall.
In advanced atherosclerosis, PM exposure can make plaques more unstable and prone to rupture. It does this by increasing the activity of enzymes that break down the plaque's protective cap (like matrix metalloproteinases or MMPs) and by promoting factors that lead to blood clotting. This increases the risk of plaque rupture, hardening of the arteries (vascular calcification), and cardiovascular events.
Conclusions
The current scientific evidence clearly demonstrates that both particulate and gaseous air pollutants can worsen atherosclerosis through harmful changes in blood fats, oxidative stress, inflammation, damage to blood vessel linings, and plaque destabilization. However, the authors noted the need for further research to address remaining uncertainties.
Future research on air pollution and atherosclerosis should focus on better ways to assess atherosclerosis in humans (such as advanced, non-invasive imaging and improved use of personal air pollution monitors to capture individual exposures).
More long-term studies are needed in diverse regions, especially in low- and middle-income countries, to understand local variations in exposure and risk. Mechanistic studies should continue to explore precisely how different pollutants affect the body at a molecular level to cause plaque formation and rupture, and identify which pollution sources and components are most harmful.
There is also a need to investigate less-studied pollutants like airborne microplastics, emissions from tire and brake wear (especially from heavier electric vehicles), and the effects of climate change on pollution mixtures. Combining findings from population studies and laboratory research will be key.
Research should also examine how air pollution interacts with other risk factors such as noise, heat, diet, and existing health conditions, and clarify how having atherosclerosis might make individuals more vulnerable to pollution. Finally, it's crucial to evaluate how effective different interventions are – from personal actions like using air purifiers or changing travel habits, to broader policies like low-emission zones – in reducing the impact of air pollution on atherosclerosis and related heart problems.