Obesity has been linked to the development of severe coronavirus disease (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). With an estimated 1.9 billion people overweight or obese worldwide, implications for the coronavirus pandemic morbidity and mortality are substantial.
A new study by researchers at the Harvard Medical School and the Ragon Institute of MGH, MIT and Harvard showed that obesity is not tied to the increased risk of SARS-CoV-2 infection. However, the team demonstrated that obesity is associated with increased manifestations of symptoms in mild COVID-19 infections, suggesting that obesity impacts the pathophysiology of COVID-19.
The study
The study released as a pre-print on the server medRxiv* highlights the risk of SARS-CoV-2 infection among obese patients. Past infections studies have shown that obese individuals, those with a body mass index (BMI) of 30 or above, are at a higher risk of being infected.
With previous viral pathogens, such as influenza A (H1N1) during the 2009 pandemic, obese people were more likely to be hospitalized, require intensive care support, and die from the infection. Obesity is also linked to a weaker immune response after natural infection of influenza or flu vaccination.
Apart from the link between obesity and clinical outcomes, evidence shows a connection between higher BMI and higher incidence of COVID-19 disease, suggesting that BMI may increase susceptibility to the infection. However, there is limited data to support this link.
To arrive at the study findings, the researchers conducted a serial serological assessment to determine the immunoepidemiology of SARS-CoV-2 infection among industry employees, comprising Space Exploration Technologies Corporation employees.
A total of 4,469 participants were enrolled in the study from work locations in California, Washington, Texas, and Florida. The duration of the study started on April 20 and ended on July 28. The researchers collected blood samples and gathered interim symptom reports every month.
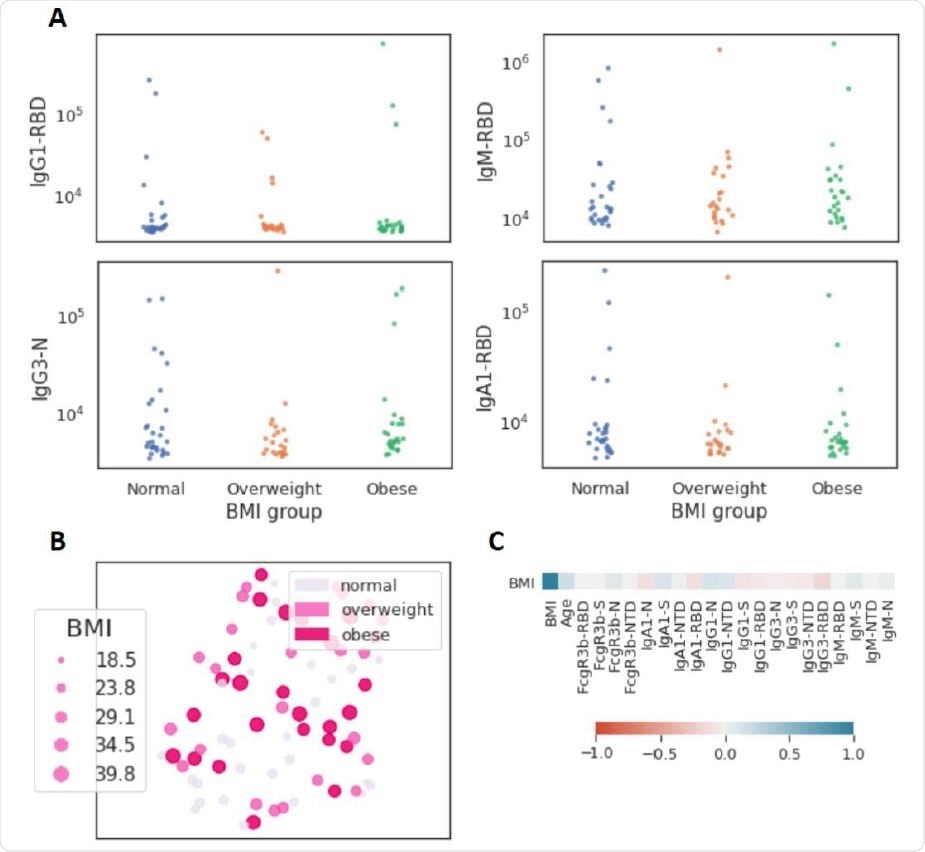
Limited influence of BMI on SARS-CoV-2 antibody profiles (n=77). (A) The dot plots show similar mean fluorescent intensity levels of IgG1, IgM, IgG3, and IgA levels across individuals classified as normal weight (n=29), overweight (n=23), and obese (n=25). (B) The uniform manifold approximation and projection (UMAP) shows the relationship between antibody profiles and BMI (dot size, color intensity), highlighting the limited influence of BMI on shaping SARS-CoV-2 antibody responses. (C) Correlation plot of shows limited correlation between BMI and 20 immunological features.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
What the study found
The researchers reported in the study that of the participants, 7.21 percent were seropositive. Obesity was tied to increased reporting of fever and other symptoms. However, there were no differences in the immune response between people of normal weight and those overweight or obese.
“We present benchmark data that obesity is not linked to increased risk of SARS-CoV-2 infection; that symptom phenotype is strongly influenced by obesity; and that despite evidence of obesity-associated immune dysregulation in severe infections,” the team explained.
“There is no evidence of muted or dysfunctional immune response across multiple immune measures among non-severe infections,” they added.
However, the team emphasized that not only are a well-established measure of severe illness like being hospitalized, being admitted to the intensive care unit, and dying from COVID-19 are more common among obese people, but obesity is also an important driver of being symptomatic in mild to moderate illness.
The study, however, has limitations. First, the study population were industry workers with over-representation, compared to the United States population as a whole. For instance, many employees were Hispanic in ethnicity, male, and younger, with fewer comorbidities, including obesity.
Obesity and COVID-19 vaccine
Health experts worry that obese people may not respond to future SARS-CoV-2 vaccines, compared to others. It has long been known that those who are obese are often unable to benefit from common vaccines, including the hepatitis B, tetanus, and influenza vaccines.
Vaccines are composed of dead virus particles or virus proteins to trigger an immune response in the body. The immune system recognizes these particles as foreign invaders, producing a protective immune response against them.
Obesity impacts the immune system in many ways, causing disrupted immune responses. Therefore, the effects of vaccination in an obese person may differ from those who are not obese.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Nilles, E., Siddiqui, S., Fischinger, S. et al. (2020). Epidemiological and immunological features of obesity and SARS-CoV-2. medRxiv. https://www.medrxiv.org/content/10.1101/2020.11.11.20229724v1
- Peer reviewed and published scientific report.
Nilles, Eric J., Sameed M. Siddiqui, Stephanie Fischinger, Yannic C. Bartsch, Michael de St. Aubin, Guohai Zhou, Matthew J. Gluck, et al. 2021. “Epidemiological and Immunological Features of Obesity and SARS-CoV-2.” Viruses 13 (11): 2235. https://doi.org/10.3390/v13112235. https://www.mdpi.com/1999-4915/13/11/2235.