Most COVID-19 patients often experience diverse neurologic complications. Further, autopsied brain tissue transcriptomic data suggest associations between severe COVID patients' cognitive decline and brain aging signatures. While recent reports implicate senescent cells in neurodegeneration and cognitive decline in aged mice and in vivo neuropathology models, their contribution to human brain tissue aging and COVID-19 pathology in the central nervous system remains unknown.
Study: Senolytic therapy alleviates physiological human brain aging and COVID-19 neuropathology. Image Credit: Jose Luis Calvo / Shutterstock
The study and findings
In the present study, researchers tested the effects of senolytics on physiological brain aging and COVID-19 neuropathology. First, they generated human brain organoids (BOs) from embryonic stem cells and physiologically aged them for eight months. Subsequently, the BOs were treated with two doses of senolytics, such as the dasatinib-quercetin (D+Q) combination, ABT-737, and navitoclax, for one month at a two-week interval.
Senolytic interventions significantly reduced senescence-associated β-galactosidase (SA-β-gal) activity, indicating the elimination of senescent cells. This was further confirmed by significantly higher levels of lamin B1 (a nuclear marker downregulated in senescence) in treated BOs. Next, the team investigated the cell types involved in senescence phenotypes by co-immunolabeling with a senescence marker (p16).
Over three-fourths of p16-positive cells coimmunostained with astrocytes (positive for glial fibrillary acidic protein), while approximately 15% co-localized with mature neurons (positive for neuronal nuclei antigen). These two brain cell populations represented a majority (> 90%) of p16-positive cells. The team found a significant reduction in senescent astrocyte populations following treatment, with the D+Q combination being the most potent. However, the effect of senolytics in reducing senescent neurons was less apparent.
RNA sequencing revealed the upregulation of lamin B1 messenger RNA (mRNA) levels across all senolytic treatments. Additionally, 81 senescence-related mRNAs were consistently suppressed with senolytic treatments. Further, aging clock predictions were performed based on whole-transcriptome sequencing. D+Q treatment of nine-month-old organoids returned their gene expression age to levels of eight-month-old organoids.
This phenotype was not observed with other tested senolytic interventions. D+Q treatment-induced changes in gene expression correlated with mammalian signatures of pro-longevity interventions, such as rapamycin administration and caloric restriction. Next, the team estimated the prevalence of senescent cells in the autopsied frontal cortex from the brains of age-matched patients who died due to severe COVID-19 or non-neurologic and non-infectious causes.
Brains of COVID-19 decedents showed over seven-fold increase in p16-positive cells than those from non-COVID-19 controls. Next, human BOs were exposed to different viral pathogens to examine how (neurotropic) viruses contribute to aging-induced neuropathology. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection was mainly detected in neurons, microglia, and neural progenitors.
Seven SARS-CoV-2 variants were also tested, and their senescence phenotypes were ranked by SA-β-gal activity. Most variants significantly increased SA-β-gal, but the Delta variant exhibited the most potent induction. Moreover, there was a distinctive colocalization of viral spike and SA-β-gal in Delta-infected BOs. Besides, a statistically higher induction of senescence was evident between organoids infected for five and 10 days.
Increased senescence observed at 10 days post-infection (dpi) relative to 5 dpi suggested that SARS-CoV-2 infection may have triggered secondary senescence. Interestingly, non-infected senescent cells were enriched within 150 µm of infected senescent cells, supporting the putative bystander effect of infected cells in triggering secondary senescence. Senescence was also triggered by infection of BOs with Japanese encephalitis virus (JEV), Zika virus (ZIKV), or Rocio virus (ROCV).
The researchers examined the associations of transcriptomic changes between COVID-19 patients and SARS-CoV-2-infected BOs. Among nearly 1,600 genes with differential expression between infected and non-infected BOs, there were 485 differentially expressed genes in COVID-19 patients' brain samples. Notably, known senescence and aging pathways were enriched in this common gene set.
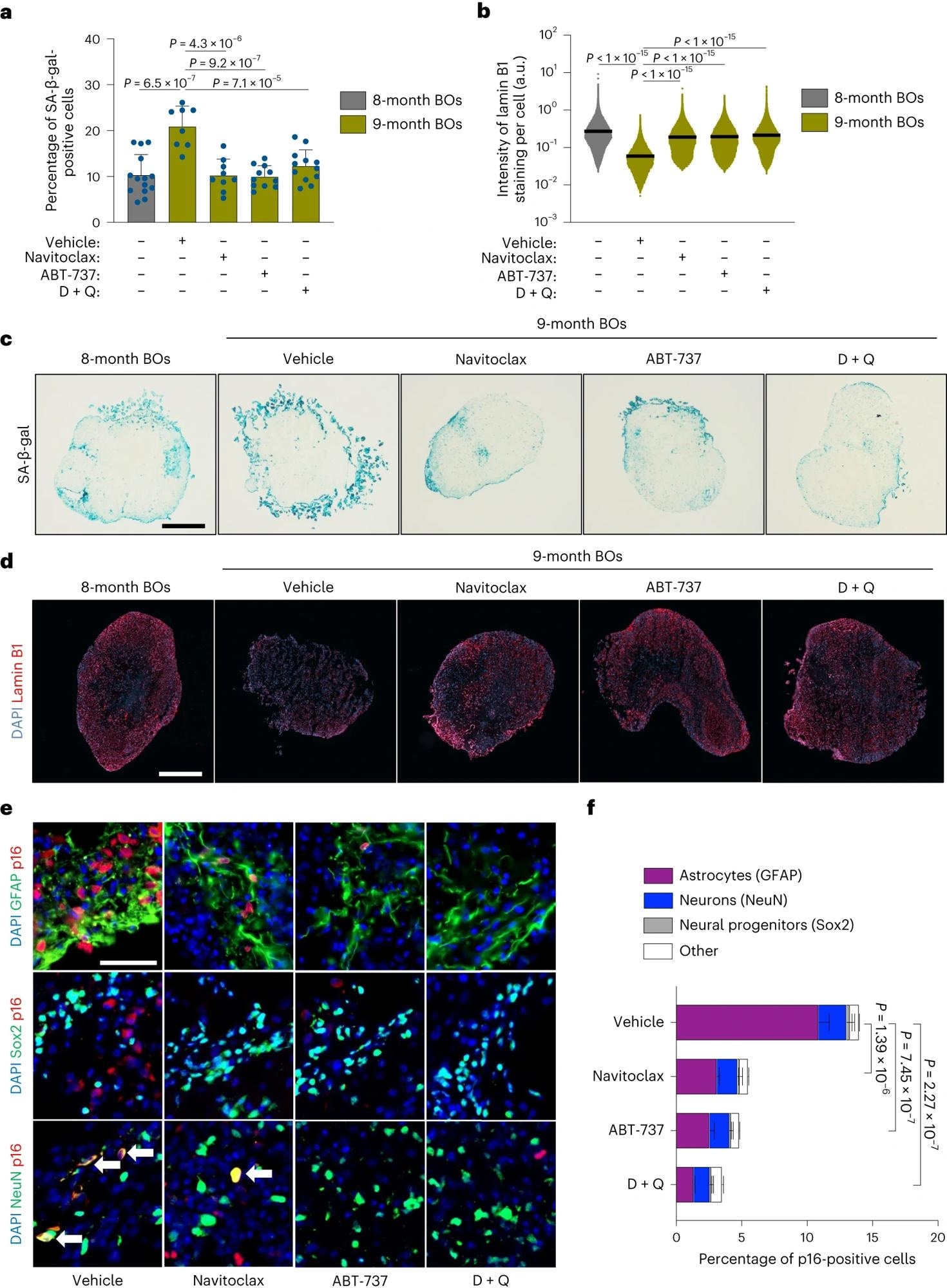 Long-term senolytic treatment prevents selective accumulation of senescent cells in physiologically aged human BOs. a–f, BOs were generated and grown in vitro for 8 months and subsequently exposed to two doses (one every 2 weeks) of either navitoclax (2.5 μM), ABT-737 (10 μM) or D + Q (D, 10 μM; Q, 25 μM) within the following month, after which organoids (n = 8–14) were collected for in situ analysis. a, SA-β-gal assay was performed on organoid sections. Each data point in the bar graph represents a single organoid analyzed. Data presented as mean ± s.d.; at least eight individual organoids were analyzed per condition; one-way analysis of variance (ANOVA) with Tukey’s multiple-comparison post hoc corrections. b, Lamin B1 staining was performed on organoid sections. Each data point in the scatter plot represents the integrated intensity of each cell within organoid sections. At least eight individual organoids were analyzed per condition; one-way ANOVA with Tukey’s multiple-comparison post hoc corrections. c,d, Representative images from quantifications shown in a,b, respectively. Scale bar, 0.3 mm. e, Representative immunofluorescent images of regions from organoids treated with the indicated senolytics and vehicle control. Samples were individually immunolabeled with antibodies against GFAP, Sox2 and NeuN and co-stained for p16. Arrows indicate coimmunoreactivity of NeuN and p16. Scale bar, 50 µm. f, Bar graphs showing colocalization quantification performed on organoid sections. Data presented as mean ± s.d.; three individual organoids were analyzed per condition; one-way ANOVA with Tukey’s multiple-comparison post hoc corrections. a.u., arbitrary units.
Long-term senolytic treatment prevents selective accumulation of senescent cells in physiologically aged human BOs. a–f, BOs were generated and grown in vitro for 8 months and subsequently exposed to two doses (one every 2 weeks) of either navitoclax (2.5 μM), ABT-737 (10 μM) or D + Q (D, 10 μM; Q, 25 μM) within the following month, after which organoids (n = 8–14) were collected for in situ analysis. a, SA-β-gal assay was performed on organoid sections. Each data point in the bar graph represents a single organoid analyzed. Data presented as mean ± s.d.; at least eight individual organoids were analyzed per condition; one-way analysis of variance (ANOVA) with Tukey’s multiple-comparison post hoc corrections. b, Lamin B1 staining was performed on organoid sections. Each data point in the scatter plot represents the integrated intensity of each cell within organoid sections. At least eight individual organoids were analyzed per condition; one-way ANOVA with Tukey’s multiple-comparison post hoc corrections. c,d, Representative images from quantifications shown in a,b, respectively. Scale bar, 0.3 mm. e, Representative immunofluorescent images of regions from organoids treated with the indicated senolytics and vehicle control. Samples were individually immunolabeled with antibodies against GFAP, Sox2 and NeuN and co-stained for p16. Arrows indicate coimmunoreactivity of NeuN and p16. Scale bar, 50 µm. f, Bar graphs showing colocalization quantification performed on organoid sections. Data presented as mean ± s.d.; three individual organoids were analyzed per condition; one-way ANOVA with Tukey’s multiple-comparison post hoc corrections. a.u., arbitrary units.
Next, the team evaluated the impact of the selective elimination of senescent cells with senolytic interventions. Senolytics significantly reduced the number of BO cells with SA-β-gal activity five days after SARS-CoV-2 infection. Of note, the impact of senolytics was more prominent in BOs infected with the Delta variant, and senolytics reverted Delta variant-induced lamin B1 loss and p21 upregulation.
Pretreating BOs with senolytics before infection resulted in a significant reduction of virus-induced senescence. Layer 6 corticothalamic neurons and gamma-aminobutyric acid (GABA)ergic ganglionic eminence neurons were the two populations with significantly higher incidence of senescence following infection, and senolytic interventions prevented cellular senescence in these populations.
Finally, the researchers infected K18-hACE2 mice (that express the human angiotensin-converting enzyme 2 [hACE2] under the regulation of keratin 18 [K18] promoter) with SARS-CoV-2 Delta. Senolytics with blood-brain barrier permeability, such as D+Q, navitoclax, and fisetin, were administered 24 hours post-infection, with subsequent treatments every two days. Infected mice had shortened life spans, with a median survival of five days.
However, fisetin or D+Q treatment significantly improved survival. All control animals died by 10 dpi, whereas 13% of navitoclax-, 38% of D+Q-, and 22% of fisetin-treated mice were alive at 12 dpi (experimental endpoint). Senolytics, especially D+Q, caused a profound decrease in COVID-19-related features and significantly reduced viral gene expression in mice brains.
The brains of infected mice exhibited an increase in inflammatory senescence-associated secretory phenotype (SASP) and p16 senescence markers, and (all) senolytic treatments normalized senescence and SASP gene expression of infected animals to the levels observed in non-infected brains. Delta infection also caused a loss of dopaminergic neurons in the brainstem, with a concomitant increase in astrogliosis. However, recurrent administration of senolytics partially prevented the loss of dopaminergic neurons and abrogated the onset of astrogliosis.
Conclusions
Taken together, the study demonstrated that senescent cells accumulate in physiologically aged human BOs, with long-term senolytic intervention(s) substantially reducing cellular senescence and inflammation. Further, D+Q treatment uniquely induced anti-aging and pro-longevity gene expression changes in BOs.
Besides, COVID-19 patients' brains exhibit rapid accumulation of cellular senescence relative to age-matched controls. Neurotropic viruses (ROCV, JEV, and ZIKV) and SARS-CoV-2 can infect BOs and induce cellular senescence, and the SARS-CoV-2 Delta variant triggers the most potent induction of senescence. Short-term senolytic interventions could reduce SARS-CoV-2 gene expression in infected BOs and prevent senescence of GABAergic and corticothalamic neurons.
Notably, senolytics ameliorated COVID-19 neuropathology in infected K18-hACE2 mice, improved their survival and clinical score, and reduced SASP, senescence, and viral gene expression. Overall, the findings highlight the vital role of cellular senescence in brain aging, COVID-19, neuropathology, and the therapeutic impact of senolytics.