New evidence shows that restoring normal glucose regulation can shield against diabetes even without weight loss, reshaping prevention strategies worldwide.

Study: Prevention of type 2 diabetes through prediabetes remission without weight loss. Image Credit: Ruslan Harutyunov / Shutterstock
In a recent Nature Medicine article, researchers investigated whether prediabetic individuals can return to normal glucose regulation despite not losing weight, often with modest weight gain, a finding that could be key to preventing type 2 diabetes (T2D).
They found that prediabetes remission occurred independently of changes in body weight and was associated with healthier fat distribution, improved β-cell function, and enhanced insulin sensitivity.
Background
T2D affects over 460 million people worldwide and is a leading cause of death because of its complications, including neuropathy, cardiovascular disease, and chronic kidney disease.
The global burden of T2D is expected to increase substantially by 2050. Poor diet quality is the primary driver, with the greatest impact in low- and middle-income countries, where access to treatment is limited. Prevention strategies are essential to reduce the worldwide burden of T2D.
Prediabetes is characterized by impaired glucose regulation or elevated HbA1c that does not meet T2D criteria. It is the most significant risk factor for T2D. The annual progression rate is 5–10%, with a lifetime risk of up to 74%.
It also independently increases the risk of vascular, cancer, and neurodegenerative diseases. Previous research has shown that restoring normal glucose regulation, even temporarily, lowers the risk of developing T2D and related complications.
Conceptually, remission here refers to normalization of glucose regulation during follow-up, not simply short-term variability. This distinction matters because transient improvements without durable metabolic change may not translate into long-term risk reduction.
About the Study
The Prediabetes Lifestyle Intervention Study (PLIS) introduced the concept of prediabetes remission. Remission is achieved when normal glucose levels are restored, often through weight loss. Such remission substantially reduces the risk of T2D and related organ damage. This emphasizes the importance of glucose regulation in preventive strategies.
Researchers conducted a post hoc analysis of PLIS, a randomized, controlled, multicenter trial conducted in Germany between 2012 and 2016. Adults aged 18–75 years with prediabetes, defined by impaired fasting glucose and/or impaired glucose tolerance, were recruited.
Participants were stratified by diabetes risk based on insulin resistance, insulin secretion, and liver fat content, and then randomized to one of three groups: a conventional lifestyle intervention, an intensified lifestyle intervention, or a control group.
For this analysis, only participants who did not lose weight over the 12-month period were included. They were classified as responders if their glucose regulation returned to normal, and as non-responders if it did not.
Focusing on the non-weight-loss subgroup isolates mechanisms beyond energy balance, helping to clarify whether tissue-specific adaptations, such as β-cell function or fat partitioning, can drive remission in the absence of weight changes.
Glucose metabolism was assessed by oral glucose tolerance tests (OGTT) with repeated blood sampling. Insulin, C-peptide, liver fat, visceral and subcutaneous fat, and muscle fat were measured using standardized assays, magnetic resonance imaging (MRI), or spectroscopy.
Additional analyses included inflammatory markers, adipokines, incretins, and genetic risk scores. Lifestyle adherence was monitored through food diaries, fitness testing, and physical activity assessments.
Findings were validated in a second cohort from the U.S. Diabetes Prevention Program (DPP), focusing on participants who also did not lose weight during the first 12 months. Statistical analyses applied mixed-effects models and corrected for multiple testing.
Key Findings
The study followed 1,105 individuals with prediabetes from the PLIS. Among the 234 participants who did not lose weight (or even gained some) during the 12-month program, 51 achieved remission while 183 did not.
Both responders and non-responders gained weight on average; however, only responders achieved remission, indicating that fat distribution and metabolic adaptation, rather than weight change itself, were decisive.
Importantly, remission occurred independently of changes in body weight, body composition, physical activity, or aerobic fitness. These improvements occurred without group differences in physical activity, aerobic capacity, or dietary adherence.
Responders showed distinct metabolic improvements. Their insulin sensitivity increased significantly, while that of non-responders remained unchanged. In addition, responders exhibited enhanced insulin secretion and improved β-cell function, changes not typically observed in weight-loss-driven remission.
Body fat distribution also differed: responders stored more fat in subcutaneous adipose tissue (SCAT) while avoiding increases in visceral adipose tissue (VAT), leading to a higher SCAT/VAT ratio. This healthier fat pattern was linked with higher adiponectin levels, which can support insulin sensitivity.
Other potential mechanisms, such as inflammation, liver fat accumulation, or genetic predisposition, did not explain remission. Notably, responders exhibited improved glucagon regulation and greater sensitivity of β-cells to glucagon-like peptide-1 (GLP-1), which supports better glucose control.
From a physiological perspective, preferential expansion of SCAT may buffer lipid overflow away from organs such as the liver and pancreas, reducing lipotoxic stress on β-cells and improving insulin action without necessitating overall weight loss.
Over the long-term follow-up, remission without weight loss reduced the risk of T2D by approximately 71%, a reduction comparable to that achieved through weight-loss-induced remission. These results were replicated in the DPP, strengthening their validity.
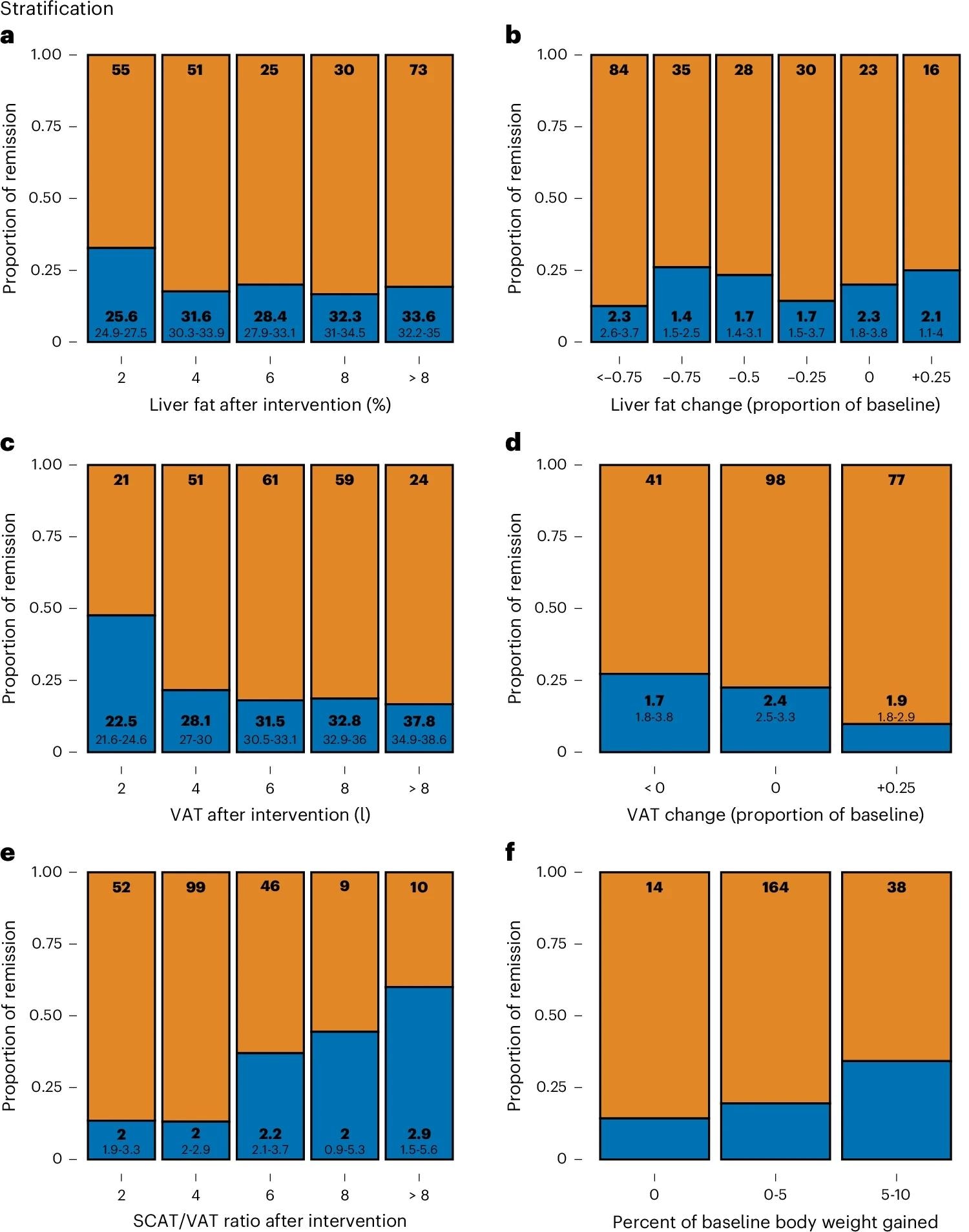
a, Stratification of R (defined by NGR, that is, prediabetes remission, after 12 months of LI, n = 51; blue) and NR (that is, not reaching NGR, n = 183) by postintervention hepatic lipid content as assessed with 1H-MRS. b, Change of hepatic lipid content during LI. c, Postintervention VAT volume as assessed with MRI. d, Change of VAT volume during LI. e, SCAT/VAT ratio. f, Change of body weight during LI. Top numbers inside the bars indicate stratum size (n). Large bottom numbers indicate BMI (a,c) or percent body weight change (b,d,e). Small bottom numbers indicate 95% CI, respectively.
Conclusions
This study demonstrates that remission of prediabetes can occur without weight loss in up to 22% of participants and provides strong protection against T2D, comparable to weight-loss-induced remission.
The key factor appears to be fat distribution: responders accumulated more subcutaneous rather than visceral fat, which was linked to greater insulin sensitivity, β-cell function, and improved GLP-1 sensitivity.
Clinically, these results suggest monitoring not only weight but also surrogate markers of visceral adiposity, such as waist circumference, and metabolic function to identify individuals likely to benefit from lifestyle interventions, even when weight plateaus.
Exercise and dietary composition may have contributed to these favorable outcomes. Importantly, the findings highlight the need to expand current clinical guidelines beyond weight loss alone, emphasizing remission to normal glucose regulation as a primary prevention target.
Strengths include replication of results in the DPP cohort and detailed metabolic profiling. Limitations are the post hoc design, reliance on surrogate OGTT measures, and potential residual confounding.
Overall, the study highlights that metabolic health and glycemic remission, rather than weight loss alone, should inform precision prevention strategies for T2D.
Journal reference:
- Sandforth, A., Arreola, E.V., Hanson, R.L., Albrechtsen, N.J.W., Holst, J.J., Ahrends, R., Coman, C., Gerst, F., Lorza-Gil, E., Cheng, Y., Sandforth, L., Katzenstein, S., Ganslmeier, M., Seissler, J., Hauner, H., Perakakis, N., Wagner, R., Machann, J., Schick, F., Peter, A., Lehmann, R., Weigert, C., Maurer, J., Preissl, H., Heni, M., Szendrödi, J., Kopf, S., Solimena, M., Schwarz, P., Blüher, M., Häring, H., Hrabé de Angelis, M., Schürmann, A., Kabisch, S., Mai, K., Pfeiffer, A.F.H., Bornstein, S., Stumvoll, M., Roden, M., Stefan, N., Fritsche, A., Birkenfeld, A.L., Jumpertz von Schwartzenberg, A. (2025). Prevention of type 2 diabetes through prediabetes remission without weight loss. Nature Medicine. DOI: 10.1038/s41591-025-03944-9, https://www.nature.com/articles/s41591-025-03944-9