A home finger-prick test promises to catch hidden cardiometabolic risks in young adults, if paired with hands-on guidance and smarter support systems.

Study: Feasibility of self-administered dried blood spot collection for cardiometabolic profile analysis in a population-based sample of young adults. Image Credit: antoniodiaz / Shutterstock
In a recent study published in the journal PLOS ONE, researchers at Deakin University in Australia examined the feasibility of self-administered dried blood spot (DBS) collection for cardiometabolic profiling in young adults.
Poor cardiometabolic health strongly predicts cardiovascular disease. Noncommunicable diseases (NCDs) are the primary cause of death in high-income countries, including Australia. Early detection of poor cardiometabolic health may help decrease the burden of NCD deaths. Young adulthood is often characterized by high-risk behaviors that negatively affect cardiometabolic health.
DBS collection kits are increasingly used for remote health screening. This method can reduce personnel, shipping, and storage costs while improving convenience, reach, and accessibility. Assays have been developed for various analytes in DBS samples, including cardiometabolic measures. However, no study has examined the feasibility of DBS collection for cardiometabolic profiling in young adults.
About the study
In the present study, researchers determined the feasibility of self-administered DBS collection for cardiometabolic profiling in young adults. The MyMeals study recruited participants between April 21 and November 21, 2022, to understand cardiometabolic health and food choices in young adults. Participants were Australian residents aged 18–30 who were not pregnant, breastfeeding, or on a vegetarian or vegan diet.
Participants were mailed a DBS collection kit and instructed to collect samples in the fasted state. Samples required at least three hours of air drying before returning. DBS samples were shipped to a laboratory for cardiometabolic profiling; this included assessment of total cholesterol (TC), triglycerides, insulin, glycated hemoglobin (HbA1c), high-sensitivity C-reactive protein (hsCRP), and high-density lipoprotein (HDL-C), low-density lipoprotein (LDL-C), and very low-density lipoprotein (VLDL-C). If blood volume was insufficient, markers were prioritized for analysis, starting with HbA1C and HDL-cholesterol.
Predefined sex- and age-relevant reference ranges were used to assess whether DBS samples were within range. Further, an online survey was administered to collect data on demographic characteristics (e.g., age, sex, education, income, relationship status, and living arrangements) and health behaviors, including physical activity, diet, smoking, sleep duration, and self-perceived health. Two survey items examined the feasibility of DBS collection.
The percentage of returned samples was calculated. Chi-squared and t-tests were performed to compare participant characteristics between those who returned an adequate sample and those who did not. Moreover, these tests were used to compare participants who provided an adequate sample to measure all eight cardiometabolic markers, regardless of whether they had difficulties collecting samples.
Findings
DBS collection kits were sent to 506 participants; of these, 366 returned samples for analysis. Among mailed kits, 69% of samples were adequate to estimate at least one cardiometabolic measure, while 46% were sufficient to measure all eight analytes. Difficulties in sample collection were reported by 72% of participants who returned their samples and 38% of those who did not return their samples.
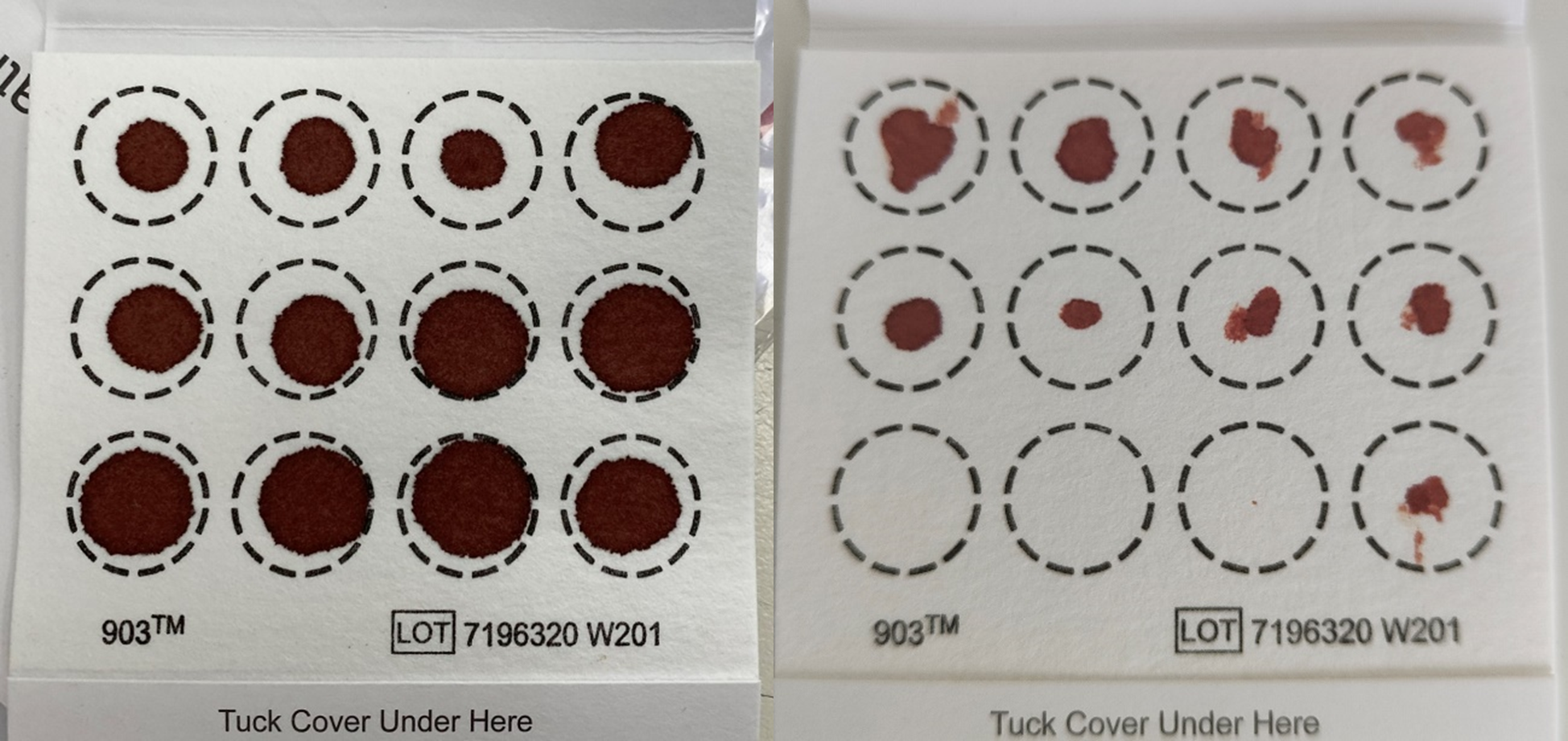
Participant dried blood spot card collection examples of A) a ‘good quality’ sample that was adequate for analysis of all eight cardiometabolic profile markers and B) a ‘poor quality’ sample that was adequate for analysis of only two cardiometabolic profile markers.
Notably, more participants without sample collection difficulties provided an adequate sample for all eight measures than those who reported difficulties. The research team noted that the high return rate was likely influenced by the intensive, personalized support they provided; researchers proactively contacted 62% of participants who were sent kits, following up with them an average of two times each (with some participants receiving up to 12 contacts).
The main challenges were a lack of blood, too few lancets —which prompted the research team to increase the number provided per kit during the study —difficulty using lancets, cold weather, and feeling overwhelmed or scared. Individuals who returned an adequate sample for all measures were aged 23.8 years, with a mean body mass index (BMI) of 26.5 kg/m².
Most participants with an adequate sample for measuring all eight markers were born in Australia (83%), had high educational attainment (56%), lived in areas of low socioeconomic disadvantage (66%), and met sleep (78%) and physical activity guidelines (66%). Further, 80% reported excellent to good health, 7% were current smokers, and 46% had a history of diabetes or heart disease.
While the authors described many characteristics as similar, the data revealed a statistically significant response bias. Participants who did not return their collection cards were significantly more likely to have a lower education status and be current smokers than those who did return a sample.
The mean TC was 187.6 mg/dL, HbA1c was 4.94%, HDL-C was 39.7 mg/dL, and LDL-C was 128 mg/dL. The median hsCRP was 0.6 mg/L, insulin was 7.93 μIU/mL, and VLDL-C was 18 mg/dL. About 74% of participants were at risk for at least one cardiometabolic marker. More males were at risk for HbA1c, insulin, and all lipid markers than females. Meanwhile, there were more females at risk for hsCRP than males.
Conclusions
The study demonstrated moderate success rates for sample adequacy but also found a statistically significant response bias. Participants who did not return an adequate sample were more likely to have a lower education status and be current smokers. The findings suggest that self-administered DBS collection is feasible but emphasize that its success highly depends on providing clear, step-by-step instructions, along with intensive, personalized, and proactive support.
Targeted approaches and practical considerations, such as providing surplus lancets, may be needed for different populations to achieve high adequacy. Notably, high proportions of participants were identified to be at risk for poor cardiometabolic health, underscoring the need for screening in young adults. However, the authors caution that these findings are not generalizable to the broader population. The study's convenience sample consisted of a higher proportion of participants with a higher socioeconomic position, and the authors explicitly state that the results cannot be generalized to lower socioeconomic groups.
Overall, the study's key takeaway is that timely and personalized support, along with clear instructions, is necessary to obtain samples of sufficient quality. Specific, practical recommendations for future studies include pilot testing collection procedures and ensuring kits contain surplus lancets to address the most common difficulty reported by participants.