Over the course of a year following the initial outbreak of COVID-19, a wide range of scientific research units and vaccine companies were able to successfully develop a number of COVID-19 vaccines.
It is possible to classify these vaccines according to their technological platforms, for example, whole virus vaccines, subunit vaccines, viral vector vaccines and gene vaccines (Figure 1).
There are currently seven vaccines that have obtained the WHO’s emergency use authorization to be used in vaccination efforts on a global scale, while more than 300 vaccines are either under development or in the pre-clinical or clinical trial stages.
This article summarizes the different classifications of COVID-19 vaccines.
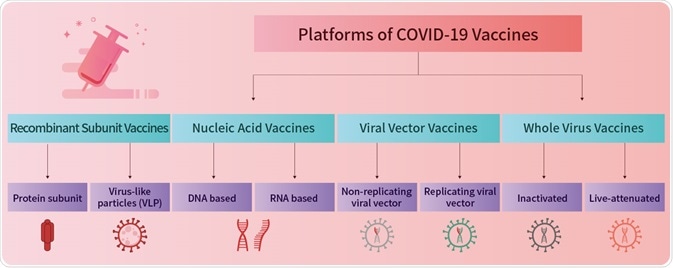
Image Credit: ACROBiosystems
Whole virus vaccines
Mechanism
Whole virus vaccines include both inactivated vaccines and live-attenuated vaccines. In this context, an inactivated vaccine is a vaccine comprised of virus particles grown in culture and killed in order to destroy their disease-producing capacity.
Live-attenuated vaccines employ still living pathogens that have been weakened, removing their ability to infect the recipient of the vaccine. The immunogenic content of whole virus vaccines neutralizes and removes the pathogen as it triggers an immune response dominated by humoral immunity or antibody-mediated immunity.
Manufacture
Whole virus vaccine pathogens are grown under highly controlled conditions. These are killed using physical or chemical methods such as heat or formaldehyde before being purified, and adjuvants are added to create vaccine preparations.
These steps increase the safety of the vaccines while preserving the structure of the antigens and maintaining their antigenicity.
Image Credit: ACROBiosystems
Features
Whole virus vaccines - particularly inactivated vaccines - exhibit a high safety profile and are well suited to large-scale production and transportation.
Their development is based on a mature technology that has been employed for hundreds of years, meaning this route towards vaccine development is often prioritized in immediate response to the outbreak of a pandemic.
The downsides of inactivated vaccines include a comparatively low level of induced immunity and the need to deliver a significant dosage for each immunization. Multiple inoculations may also be required to generate sufficient protection.
Representative products
BBIBP-CorV (Sinopharm, China): This vaccine offers 78% protection against symptomatic infections while being 100% effective against severe diseases.
CoronaVac (Sinovac, China): This vaccine offers around 66% protection against symptomatic infections while being 90% effective against severe diseases.
Both BBIBP-CorV and CoronaVac have been approved for use by the WHO. These vaccines have been employed in large-scale vaccination efforts in Africa, Asia, South America and Europe.
India, Russia, Kazakhstan and Iran have also developed inactivated vaccines for COVID-19. These have been approved by at least one governmental health sector for use in the general population.
Data retrieved from the McGill COVID19 Vaccine Tracker suggests that more than 20 inactivated vaccines are currently under development or at the clinical trial stage.
Subunit vaccines
Mechanism
Subunit vaccines only include selected antigenic parts such as fragments of the virus’ proteins. This differs from whole virus vaccines, which contain the whole pathogen.
Certain subunit vaccines make use of virus-like particles (VLPs) - proteins assembled into the natural shape of the virus’ outer shell in order to mimic genuine virus particles.

Image Credit: ACROBiosystems
Manufacture
The production of subunit vaccines involves recombinantly expressing and collecting viral antigens in vitro. To do this, an expression vector including the target antigen gene is transfected into engineered cell lines designed to express large quantities of the target protein.
This protein is then purified, with adjuvants added to create vaccines preparations.
Features
As subunit vaccines do not contain ‘live’ pathogen components, there is no danger of the vaccine introducing the disease. Subunit vaccines are, therefore, safer and more stable than vaccines containing whole pathogens.
Subunit vaccines are based on well-established technology, as well as being well suited for use with immunocompromised patients.
Their disadvantages include relatively complex manufacturing processes versus other vaccines such as mRNA vaccines. They may also necessitate the use of adjuvants and booster shots, with extra time taken to determine which antigenic combinations work best.
Representative products
ZF2001 (Anhui Zhifei Longcom, China): This vaccine employed RBD-Dimer as its main antigenic component.
NVX-CoV2373 (Novavax, USA): This vaccine employs a full-length spike trimer as its antigenic component.
A significant number of COVID-19 vaccines are based on the recombinant subunit development route.
Overall protection by subunit vaccines in clinical trials has been found to be higher than that of inactivated whole virus vaccines. More than 50 protein subunit vaccines are currently under development.
Viral vector vaccines
Mechanism
Viral vector vaccines leverage a modified version of one virus as a vector in order to deliver specific genetic material coding for the targeted antigen of another infectious agent. This is delivered into the recipient’s host cells.
It is important to note that neither the virus used as the vector nor the source of the antigen causes infection, but the delivered genetic material enables antigen expression within cells.
This material is also able to induce a strong cytotoxic T cell response, in contrast to subunit vaccines which will only confer humoral immunity.

Image Credit: ACROBiosystems
Manufacture
The production of viral vector vaccines involves the construction of a viral vector containing the target antigen gene. The majority of viral vectors are specifically designed to be incapable of replication since the necessary genes for this are removed.
Features
The adenovirus vector is the most commonly utilized viral vector, largely due to its capacity for transgene expression, high transduction efficiency, broad viral tropism and its ability to infect dividing and non-dividing cells.
One notable disadvantage is that many people have developed pre-existing immunity to adenoviruses from previous exposures. Human adenovirus serotype 5 is generally used because this can be easily produced in high titers.
Representative products
Ad26.COV2.S (Janssen (Johnson & Johnson), USA): This vaccine offers 85% universal protection as well as 100% protection against severe diseases
AZD1222 (Oxford/AstraZeneca, UK): This vaccine offers around 81% protection against wild-type virus and Alpha mutant strains.
Ad5-nCoV (CanSino Biologics, China): This vaccine offers 66% universal protection as well as 91% protection against severe illness.
Three different viral vector vaccines have been approved by the WHO: Ad26.COV2.S (Johnson & Johnson), AZD1222 (Oxford/AstraZeneca) and Covishield (Oxford/AstraZeneca formulation).
Clinical trials are still underway for over 30 viral vector vaccines.
Gene vaccines
Mechanism
Gene vaccines work by introducing a specific antigen-coding DNA or mRNA sequence into an organism’s cells in order to induce an immune response.
Antigen can be synthesized from genetic material via the host cells’ expression system, prompting the host to develop a strong immune response to the antigen protein. This helps to both prevent and treat diseases.

Image Credit: ACROBiosystems
Manufacture
Production of gene vaccines necessitates a process of molecular sequence design and in vitro transcription followed by purification of the genetic molecules and the mixing of these with delivery molecules.
The mRNA in mRNA vaccines is delivered via a co-formulation of RNA encapsulated in lipid nanoparticles. These nanoparticles help protect the RNA strands and support their absorption into cells.
Features
Gene vaccines offer a number of advantages over traditional vaccines, including easier design, rapid manufacture and comparatively low production costs. Gene vaccines also benefit from the capacity to induce both cellular and humoral immunity.
Their key disadvantage is that some mRNA vaccines require ultracold storage prior to distribution. Work is ongoing to mitigate this downside, however.
Representative products
mRNA-1273 (Moderna, USA): This vaccine offers between 94% and 100% protection against the moderate to severe symptoms caused by various VOCs (except Delta). Protection remains high (93%) 6 months after inoculation.
BNT162b2 (Pfizer/BioNTech): This vaccine offers 97% protection against severe diseases, reducing to around 91% six months after inoculation.
ZyCoV-D (Cadila Healthcare, India): This is the first DNA vaccine that was approved for use with humans, having been given emergency approval by Indian authorities in August of 2021.
The WHO has since approved the mRNA-1273 (Moderna, USA) and BNT162b2 (Pfizer/BioNTech), using these as part of large-scale vaccination efforts around the world. Both of these vaccines have been confirmed to offer high effectiveness.
There are currently more than 30 COVID-19 mRNA vaccines in pre-clinical or clinical trials. For example, in China, the ARCoV mRNA vaccine jointly developed by Walvax Biotechnology, Suzhou Abogen Biosciences and the PLA Academy of Military Science is undergoing a phase 3 clinical trial.
A summary of different COVID-19 vaccines
Source: ACROBiosystems
| Technology |
Antigen |
Pros |
Cons |
Representative products |
| Whole Virus Vaccines |
Inactivated Vaccines |
Killed SARS-CoV-2 virus |
- High safety profile
- Easy to produce and transport on a large scale
|
- Relatively low level of induced immunity
- Large dosage required for each immunization
- Multiple inoculations may be required
|
BBIBP-CorV-Sinopharm (Beijing)
CoronaVac- Sinovac
Covaxin- Bharat Biotech
KoviVac- Chumakov Center
|
| Live-Attenuated Vaccines |
Live but weakened SARS-CoV-2 virus |
- Strong immunogenicity that induces long-lasting immunity
|
- Not suitable for immune-suppressive individuals
|
DelNS1-nCoV-RBD LAIV- The University of Hong Kong
MV-014-212- Meissa Vaccines Inc
COVI-VAC- Codagenix Inc
|
| Subunit Vaccines |
Protein Subunit Vaccines |
Fragments of spike antigens |
- High safety profile
- Efficient for mass production
|
- Relatively low level of induced immunity
- Short term immunity that requires repeated inoculations
|
RBD-Dimer- Anhui Zhifei Longcom
NVX-CoV2373- Novavax
EpiVacCorona- FBRI
|
| VLP Vaccines |
VLPs ensembled from fragments of antigens |
- High bioactivity
- Strong immunogenicity that induces high titers of antibody
|
- of virus due to packaging difficulty
|
Medicago Plant-based VLP
|
| Viral Vector Vaccines |
Another viral vector containing genes coding SARS-CoV-2 spike antigens |
- Safe and effective
- Suitable for multi-valent vaccine development
- Can induce cellular immunity
|
- Effectiveness might be compromised by pre-existing immunity to adenoviruses
|
Ad26.COV2.S- Janssen (Johnson & Johnson)
AZD1222- Oxford/AstraZeneca
Covishield- Serum Institute of India
Ad5-nCoV- CanSino
Sputnik V, Sputnik Light- Gamaleya
|
| Gene Vaccines(DNA/RNA) |
DNA or mRNA coding SARS-CoV-2 spike antigens |
- Simple and fast to design in response to virus outbreaks
- Induce both humoral and cell-mediated immunity
|
- Some vaccines require cold-chain storage and supply
- Long term effects need to be evaluated
|
mRNA-1273- Moderna
BNT162b2- Pfizer/BioNTech
ZyCoV-D- Zydus Cadila
|
About ACROBiosystems
ACROBiosystems is a cornerstone enterprise of the pharmaceutical and biotechnology industries. Their mission is to help overcome challenges with innovative tools and solutions from discovery to the clinic. They supply life science tools designed to be used in discovery research and scalable to the clinical phase and beyond. By consistently adapting to new regulatory challenges and guidelines, ACROBiosystems delivers solutions, whether it comes through recombinant proteins, antibodies, assay kits, GMP-grade reagents, or custom services. ACROBiosystems empower scientists and engineers dedicated towards innovation to simplify and accelerate the development of new, better, and more affordable medicine.
Sponsored Content Policy: News-Medical.net publishes articles and related content that may be derived from sources where we have existing commercial relationships, provided such content adds value to the core editorial ethos of News-Medical.Net which is to educate and inform site visitors interested in medical research, science, medical devices and treatments.